In a world where cancer remains one of the most formidable health challenges, groundbreaking research is shedding light on innovative ways to harness the body’s own defenses to combat this disease and improve patient outcomes. Recent studies have unveiled a promising strategy that focuses on transforming the immune system’s response to tumors, potentially preventing recurrence and enhancing survival rates. This approach, rooted in cutting-edge immunology, targets tumors that typically evade immune detection, turning them into battlegrounds where the body’s natural fighters can thrive. By re-engineering the environment within tumors, scientists are paving the way for therapies that could redefine cancer treatment. This development not only offers hope to millions but also underscores the importance of immunity as a cornerstone in the fight against malignancy. As research progresses, the implications of these findings could ripple across oncology, offering a glimpse into a future where cancer is met with a fortified immune response, ready to strike at its core.
Revolutionizing Tumor Environments with Immune Activation
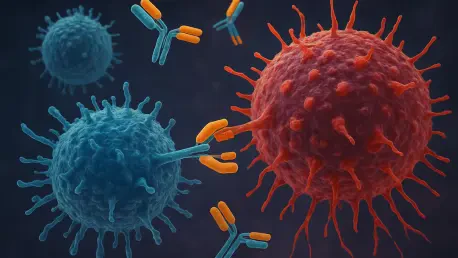
A pivotal aspect of recent cancer research centers on altering the landscape within tumors to make them more recognizable to the immune system. Many tumors are classified as “immune-cold,” meaning they effectively hide from immune detection, leading to poor treatment outcomes. Scientists have developed a novel method to convert these elusive tumors into “immune-hot” ones by introducing specific immune-activating agents. This transformation involves stimulating the formation of tertiary lymphoid structures (TLSs), which are clusters of immune cells associated with improved responses to therapy. By targeting specific proteins with dual agonists, researchers have observed a rapid mobilization of killer T cells, which play a critical role in attacking cancer cells. This approach has shown remarkable success in preclinical models across various cancer types, including breast and pancreatic, highlighting its potential to shift the paradigm of how resistant tumors are addressed in clinical settings.
Beyond the initial activation, this strategy fosters a sustainable immune response by facilitating the development of specialized blood vessels within tumors. These vessels act as entry points for a large influx of immune cells, enabling the assembly of TLSs where both T cells and B cells can mature and coordinate their attack. The presence of these structures has been linked to the production of tumor-specific antibodies and long-lived memory cells, which are essential for preventing cancer from returning. Moreover, the persistence of certain immune cells in the bone marrow suggests that this method could establish a systemic defense mechanism, offering protection against relapse. This comprehensive immune engagement not only targets existing tumors but also builds a foundation for long-term vigilance, addressing one of the most persistent challenges in cancer care. As such, the ability to engineer an immune-friendly tumor environment represents a significant leap forward in enhancing patient outcomes.
Enhancing Treatment Synergies through Immune Strategies
Another compelling dimension of this research lies in its potential to complement existing cancer therapies. By amplifying the immune system’s capabilities, the dual-activation approach could significantly boost the effectiveness of treatments like checkpoint inhibitors and chemotherapy, which often struggle against immune-cold tumors. The correlation between TLS abundance and better survival rates across various cancer types suggests that integrating immune activation into standard protocols might improve results for a wide range of patients. This synergy could be particularly impactful for those with historically poor prognoses, offering a renewed chance at remission. Researchers are optimistic that combining these immune-enhancing techniques with conventional methods will create a more robust anti-cancer arsenal, capable of tackling even the most stubborn malignancies with precision.
Further exploration into this strategy reveals its adaptability across diverse tumor profiles, underscoring its broad applicability. The balanced activation of both humoral and cell-mediated immunity ensures a multifaceted attack on cancer cells, reducing the likelihood of resistance. Helper T cells and memory cells play a crucial role in sustaining this response, amplifying the body’s natural defenses over time. This balanced immune signaling not only directly combats tumors but also fortifies the system against future threats, creating a self-reinforcing cycle of protection. As studies continue to refine these methods, the prospect of tailoring immune activation to individual patient needs becomes increasingly feasible. This personalized approach could address the unique challenges posed by different cancer types, ensuring that therapies are as effective as possible. The ongoing work to translate these findings into clinical applications holds immense promise for transforming how cancer is managed in the years ahead.
Paving the Way for Future Innovations in Cancer Care
Looking back, the strides made in re-engineering the tumor microenvironment through immune activation marked a turning point in oncology. The meticulous efforts to induce TLS formation and foster a robust immune response in preclinical models demonstrated tangible success in inhibiting tumor growth. These early interventions established a precedent for creating a self-sustaining anti-cancer environment, one that offered enduring protection against recurrence. Reflecting on these achievements, it became clear that the nuanced interplay between T cells and B cells was instrumental in crafting a comprehensive defense strategy, setting a high standard for future research.
Moving forward, the focus shifts to translating these preclinical triumphs into real-world benefits for patients. The path ahead involves rigorous clinical trials to validate the efficacy of TLS therapy across diverse populations, addressing the limitations of current treatments for immune-cold tumors. Continued investigation into the mechanisms behind immune activation promises to uncover new insights, potentially unlocking further therapeutic avenues. As the field of immunotherapy evolves, the emphasis on building a resilient immune infrastructure within tumors remains a guiding principle, inspiring hope for improved survival rates. This journey, grounded in innovation, highlights the critical need to sustain momentum in exploring how the body’s defenses can be harnessed to outsmart cancer at every turn.