Alcohol consumption, particularly chronic or heavy usage, has long been identified as a significant health risk, impacting various bodily systems and functions. Recent research, particularly the review published in “Metabolites,” delves into the intricate relationship between alcohol intake and male metabolic health and fertility. Researchers in Italy have specifically analyzed how alcohol disrupts liver function, lipid metabolism, and testosterone production, contributing to a range of health issues.
Alcohol and Metabolic Health
Alcohol Metabolism
Upon ingestion, alcohol is absorbed in the stomach and small intestine and then processed in the liver, primarily through oxidative and non-oxidative pathways. The oxidative pathway involves enzymes like alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH), which convert alcohol into acetaldehyde and acetate. This process generates reactive oxygen species (ROS), contributing to oxidative stress and inflammation. Non-oxidative pathways produce metabolites such as fatty acid ethyl esters and phosphatidylethanol. The efficiency of these pathways can vary significantly due to genetic factors, diet, comorbidities, and drinking patterns.
Oxidative stress generated during alcohol metabolism has profound implications on overall metabolic health. The resultant inflammation further exacerbates the impairment caused to metabolic pathways, contributing to broad spectrum metabolic dysfunction. It’s crucial to note that genetic predispositions can make some individuals more susceptible to these detrimental effects. Moreover, factors such as one’s diet and other existing health conditions can further influence how the body reacts to alcohol, making personalized healthcare and recommendations critical in managing alcohol consumption effectively.
Liver Dysfunction
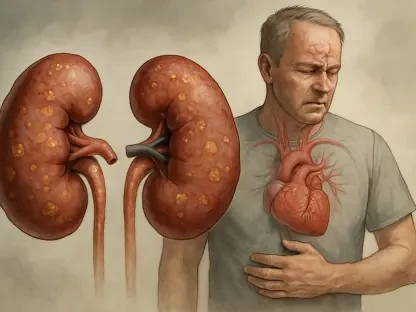
Overconsumption of alcohol is linked to a spectrum of liver diseases, from reversible fatty liver to severe conditions such as alcoholic hepatitis, cirrhosis, and hepatocellular carcinoma. Chronic alcohol intake disrupts liver function through mechanisms including excess acetaldehyde production, oxidative stress, impaired lipid metabolism, and apoptosis. Additionally, alcohol alters gut microbiota balance and increases intestinal permeability, leading to elevated levels of lipopolysaccharide (LPS) that activate immune cells and promote liver apoptosis.
This hepatic disruption is particularly concerning as the liver plays a pivotal role in multiple metabolic processes. When liver function is compromised, the body’s ability to manage lipid metabolism and detoxification is significantly impaired. This can lead to an accumulation of fat in the liver cells, known as steatosis, which is the hallmark of fatty liver disease. The progression from steatosis to more severe alcoholic liver diseases such as hepatitis and cirrhosis involves chronic inflammation, cellular damage, and fibrosis, ultimately culminating in liver failure if left unchecked. The alteration in gut microbiota and increased intestinal permeability forms a vicious cycle that perpetuates liver damage, highlighting the interconnected nature of bodily systems.
Impact on Metabolic Syndrome and Diabetes
Alcohol affects insulin resistance, mitochondrial function, and oxidative stress, disrupting lipid metabolism and enhancing inflammation. While light-to-moderate drinking might reduce the risk of type 2 diabetes (T2D), heavy alcohol use exacerbates metabolic dysfunction and liver damage through impaired insulin signaling and oxidative stress. The link between chronic alcohol consumption and metabolic syndrome, characterized by a cluster of conditions such as hypertension, hyperglycemia, excess abdominal fat, and abnormal cholesterol levels, further illustrates alcohol’s far-reaching impact on health.
Heavy alcohol consumption exacerbates these metabolic disturbances, leading to increased risk of developing conditions such as type 2 diabetes and metabolic syndrome. This happens through multiple mechanisms, including impaired insulin signaling, which is crucial for regulating blood sugar levels. The combination of increased oxidative stress and inflammation adds to the cellular damage seen in individuals with chronic alcohol intake, leading to a cycle of metabolic impairment that is difficult to reverse. On a molecular level, disrupted lipid metabolism affects the balance between lipid storage and oxidation, contributing to widespread metabolic complications.
Alcohol’s Effect on Testosterone Production
Acute and Chronic Impacts
Alcohol consumption impacts testosterone production through complex mechanisms. Acute intake can lower testosterone levels by depleting NAD+, suppressing gonadotropins, and disrupting steroidogenesis, affecting the hypothalamic-pituitary-gonadal (HPG) axis. Chronic alcohol use generally reduces testosterone levels, influenced by liver damage and hormonal imbalances, such as elevated estrogen levels. A meta-analysis of chronic alcohol users showed a reduction in serum testosterone by about 4.86 nmol/L compared to non-users.
These hormonal disruptions have significant implications for male reproductive health and general well-being. Acute impacts may cause temporary drops in testosterone, but chronic alcohol use can lead to sustained low levels of the hormone, resulting in long-term consequences. The depletion of NAD+ and suppression of gonadotropins disrupt key processes in hormone synthesis, further compounded by liver damage from prolonged alcohol consumption. Additionally, an increase in estrogen levels due to liver dysfunction can create further hormonal imbalances, exacerbating the adverse effects on testosterone production and overall male reproductive health.
Adolescent Health
The effects of alcohol on testosterone production during adolescence, a pivotal development stage, are not well understood. This highlights a major research gap that needs addressing to understand the long-term reproductive health implications for younger populations. Adolescence is a critical period for hormonal development, and disruptions caused by alcohol can lead to long-term reproductive health issues. This age group is particularly vulnerable because their bodies are still developing, and early exposure to alcohol could set a precedent for future health complications.
Understanding these impacts is crucial for developing targeted public health strategies aimed at reducing alcohol consumption among adolescents. As their hormonal systems are still maturing, they might be more susceptible to long-lasting effects from alcohol exposure, potentially leading to reproductive health challenges later in life. Hence, filling this research gap is essential in shaping informed guidelines and preventive measures to protect the reproductive health of younger individuals who are at a critical stage of their development.
Alcohol’s Impact on Male Reproductive Health
Spermatogenesis
Alcohol intake, particularly chronic use, adversely affects male fertility with notable impacts on spermatogenesis. Acute alcohol consumption raises oxidative stress and impairs Sertoli cell function, disrupting sperm production. Chronic use has more severe effects, reducing semen quality, including sperm volume, concentration, and morphology. Severe cases can lead to conditions such as spermatogenic arrest and Sertoli-cell-only syndrome, although some damage might be reversible with the cessation of alcohol intake.
These adverse effects on spermatogenesis can significantly impair male fertility and lead to challenges in conceiving. The intricate processes involved in sperm production are highly sensitive to disruptions caused by oxidative stress and impaired Sertoli cell function, elements directly impacted by alcohol intake. Chronic alcohol consumption amplifies these issues, leading to decreased semen quality and potential infertility. However, it’s worth noting that cessation of alcohol intake may allow for partial recovery of sperm production, highlighting the body’s resilience and ability to heal when given the opportunity to abstain from harmful substances.
Confounding Factors
Research into alcohol’s impact on fertility is often complicated by confounding factors such as smoking, drug use, and comorbid health conditions, making it challenging to draw definitive conclusions. These additional variables can skew study results, making it difficult to isolate alcohol’s specific impact on male fertility. This complexity underscores the importance of comprehensive research methodologies that account for these confounding factors to yield more accurate, reliable findings.
Understanding the full extent of alcohol’s impact on male fertility requires disentangling these myriad influences. Researchers need to carefully design studies that minimize the effects of these confounding variables to authentically capture the relationship between alcohol consumption and reproductive health. By addressing these complexities, future research can provide clearer insights and more actionable recommendations for individuals and healthcare providers alike, aiming to improve reproductive health outcomes by reducing or eliminating alcohol consumption.
Public Health Implications
Differential Impacts of Alcohol Consumption
The review calls for a nuanced understanding of the differential impacts of acute, moderate, and chronic alcohol consumption. Public health strategies need to recognize these distinctions to formulate more effective clinical recommendations and preventive measures. It’s crucial to comprehend that while some studies suggest potential antioxidant benefits of light-to-moderate drinking, chronic heavy use poses significant risks that outweigh any potential advantages. Differentiating between these levels of alcohol consumption can help create more targeted strategies for public health interventions and education.
Formulating effective public health policies requires acknowledging the different facets of alcohol consumption and their respective impacts. By distinguishing the varying effects of acute, moderate, and chronic intake, health authorities and professionals can provide more informed and relevant advice to the public. This approach can lead to the development of guidelines that cater to individual needs and circumstances, promoting healthier lifestyle choices and mitigating the risk of alcohol-related health issues.
Need for Ongoing Research
Alcohol consumption, especially when chronic or heavy, is well-known as a major health risk, affecting several bodily systems and their functions. It has a particularly adverse impact on male metabolic health and fertility, as explored in a recent review published in “Metabolites.” Researchers in Italy have examined the specific ways in which alcohol interferes with liver function, lipid metabolism, and testosterone production, leading to numerous health problems.
According to the study, alcohol-induced liver damage is a critical factor, as the liver plays a vital role in regulating metabolism and detoxifying the blood. Chronic alcohol intake disrupts this process, leading to the accumulation of harmful substances in the liver and bloodstream. Additionally, alcohol alters lipid metabolism, increasing the levels of unhealthy fats and leading to cardiovascular issues. The research also highlights that alcohol consumption significantly reduces testosterone levels, which can impair male fertility and cause other hormonal imbalances.
Overall, the findings stress the critical need to understand the full extent of alcohol’s effects on men’s health, underlining the importance of moderation or abstinence.