In a landmark decision that reshapes the landscape of healthcare in Spain, the Council of Ministers has approved a Royal Decree on October 7, ushering in the regulated use of cannabis-based medicines within hospital settings, marking a historic shift toward integrating medical cannabis into the nation’s healthcare framework. This long-anticipated move, celebrated by patients, activists, and medical professionals alike, signals a profound change in policy. Spearheaded by the Ministry of Health, the regulation introduces stringent guidelines for prescribing and dispensing standardized cannabis oils, ensuring a balance between innovation and patient safety. After years of advocacy and stalled progress, this decree not only acknowledges the therapeutic potential of cannabis but also sets a precedent for evidence-based treatment options. It marks a critical juncture for thousands of patients seeking alternative therapies, while sparking discussions on accessibility and implementation challenges that lie ahead.
A New Era of Medical Oversight
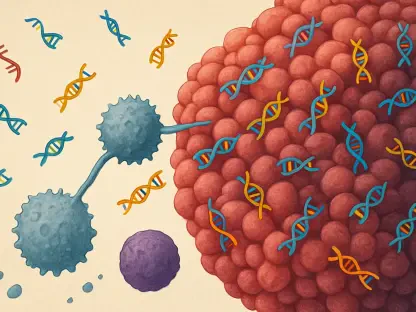
The newly enacted Royal Decree establishes a tightly controlled framework for the use of cannabis-based medicines, limiting prescriptions to specialist physicians operating within hospital environments. This regulation explicitly excludes the use of cannabis flower, focusing solely on standardized oils as the approved form of treatment. The Spanish Agency of Medicines and Medical Devices (AEMPS) has been tasked with developing comprehensive monographs within a three-month period, detailing clinical applications, preparation standards, dosage guidelines, and specific prescribing conditions. Such a structured approach underscores Spain’s dedication to ensuring safety and efficacy in medical cannabis use. Moreover, the framework is designed with adaptability in mind, allowing for updates as new scientific evidence emerges, which positions the country at the forefront of cautious yet progressive medical innovation in this field.
Beyond the technical specifics, the regulatory scope reflects a deliberate effort to prioritize patient safety while navigating the complexities of introducing a controversial treatment into mainstream healthcare. By confining prescriptions to hospital settings and specialist oversight, the decree aims to mitigate risks of misuse or inconsistent application across diverse medical contexts. This careful calibration also serves as a response to global debates on how best to integrate cannabis into medical systems without compromising public health standards. While this initial step is narrow in scope, it lays a robust foundation for potential expansion, provided that ongoing research and clinical outcomes support broader applications. The emphasis on evidence-based updates through AEMPS monographs ensures that the regulation remains dynamic, capable of evolving with advancements in medical understanding.
Ensuring Equitable Access for Patients
A cornerstone of this groundbreaking regulation is its commitment to equitable access, particularly through the provision that patients will not incur costs for prescriptions dispensed via hospital pharmacies. This financial relief sets Spain apart from many other nations where economic barriers often impede access to medical cannabis treatments. Although the prescribing authority rests solely with hospital-based specialists, the framework includes exceptions for remote dispensing in cases of vulnerability, dependency, or geographical isolation. These measures aim to address disparities in access, ensuring that patients in remote or underserved areas are not left behind in benefiting from this new therapeutic option. The focus on cost-free access highlights a patient-centric approach rarely seen in similar international programs.
Equally significant is the potential impact on patient quality of life, as this regulation opens doors for individuals who have long sought alternative treatments for chronic conditions. The removal of financial hurdles through hospital pharmacy dispensing means that economic status will not dictate who can benefit from cannabis-based therapies, a progressive stance that could serve as a model for other countries. However, the limitation to hospital settings raises questions about whether access will truly be as inclusive as intended, especially for those unable to travel to such facilities regularly. Despite these concerns, the inclusion of remote dispensing provisions offers a pragmatic solution to bridge gaps, reflecting a nuanced balance between strict oversight and the practical realities of patient needs across diverse regions.
The Long Road of Advocacy
The journey to this historic regulation has been marked by over a decade of persistent advocacy from patients, families, and healthcare professionals who championed the recognition of cannabis as a legitimate medical resource. Key milestones, such as the Health Committee’s recommendations several years ago, laid critical groundwork for this moment, though progress often faced delays due to political and systemic challenges. Patient activist Carola Pérez has emerged as a prominent voice in this movement, describing the decree as a monumental victory for thousands who have endured years of struggle to access compassionate care. Her perspective emphasizes that while this achievement is significant, it represents only the beginning of a broader mission to normalize and expand medical cannabis options in Spain.
Reflecting on the historical significance of this decree, it becomes clear that the power of grassroots advocacy cannot be understated in driving systemic change within healthcare policy. The voices of patients sharing personal testimonies, alongside the persistent efforts of medical professionals advocating for evidence-based alternatives, have collectively shifted public and governmental perceptions over time. This regulation stands as a testament to their resilience, proving that sustained collective action can influence even the most entrenched systems. Yet, as Pérez and others note, the fight is far from over, with ongoing advocacy needed to address the current framework’s limitations and ensure that the evolving needs of patients remain at the forefront of policy discussions.
Navigating Implementation Hurdles
Despite widespread celebration of this regulatory milestone, significant concerns persist regarding the practical challenges of implementation and the restrictive nature of the current framework. Critics highlight limitations such as the exclusion of cannabis flower and the confinement of dispensing to hospital pharmacies, which could restrict access for many patients who might benefit from broader options or more convenient distribution channels. Additionally, the readiness of healthcare professionals to adopt this new system is under scrutiny, with many lacking sufficient training in prescribing cannabis-based medicines. This gap in expertise could lead to delays or inconsistencies in patient care, underscoring the urgent need for comprehensive education programs.
Further complicating the rollout is the necessity for uniform application across Spain’s diverse regions to prevent the issue from becoming politicized rather than driven by scientific consensus. High anticipated demand from patients adds another layer of pressure, requiring swift coordination between healthcare providers, regulatory bodies, and regional authorities to ensure seamless delivery of care. While the regulation’s design allows for future updates through AEMPS guidelines, the immediate focus must be on equipping medical staff with the knowledge and resources needed to meet patient needs effectively. Addressing these hurdles will be crucial in determining whether this historic step fulfills its promise of transforming patient access to innovative therapies or falls short due to logistical and structural barriers.