New Zealand faces an urgent challenge in addressing the mental health needs of older adults with dementia, particularly those exhibiting psychiatric symptoms. Despite comprehensive recognition of the nation’s mental health crisis through inquiries like He Ara Oranga, a glaring gap persists in support for dementia patients requiring psychiatric care. This deficiency places these vulnerable individuals, as well as healthcare providers, at risk. The ongoing practice of admitting these patients to general medical wards, lacking specialized psychiatric resources and training, exacerbates the situation. New Zealand’s healthcare infrastructure struggles to meet the demand for psycho-geriatric facilities, as seen in the dwindling number of specialized beds, particularly acute in regions like Dunedin. As the population ages and the need for adept psychiatric interventions grows, a reevaluation of current practices is vital to ensuring the safety and dignity of all stakeholders.
Inappropriate Ward Placements and Their Consequences
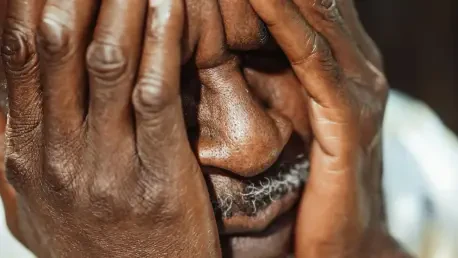
Impact on Dementia Patients
Dementia patients experiencing Behavioral and Psychiatric Symptoms of Dementia (BPSD) face significant challenges when admitted to general medical wards not equipped for their needs. Lacking amenities such as single rooms for patient security and low-stimulus environments can exacerbate distress symptoms. Exposure to constant light, noise, and inappropriate interventions may lead to heightened anxiety, agitation, and even aggression. Care in these settings often fails to meet the New Zealand Code of Health and Disability Services Consumers’ Rights, which mandates adequate standards of care. Furthermore, the absence of specialized care compromises the potential for effective management and treatment, severely impacting their quality of life.
Medical personnel in these wards often lack the specialized training necessary to manage dementia-related aggression and complex behaviors, increasing the risk of adverse incidents. Incidents of misunderstanding or mismanagement of these symptoms can lead to situations where the safety of both patients and staff is jeopardized. This lack of preparedness is particularly problematic when dealing with potentially violent behaviors that require careful, informed management. Without appropriate resources or trained staff, healthcare environments can become places of risk instead of care, highlighting the need for specialized psychiatric resources dedicated to dementia care.
Safety Concerns for Healthcare Staff
Staff safety is another critical concern when dementia patients with psychiatric needs are placed in unsuitable medical wards. Healthcare workers, including nurses and aides, often confront situations involving physical aggression without the requisite training or support to manage these incidents safely. The absence of secure units or restraint options can turn these encounters hazardous. Additionally, when dealing with violent behaviors, female staff members are particularly vulnerable, raising significant ethical and professional concerns regarding their working conditions. Ensuring that healthcare environments are equipped with both physical and procedural measures to protect staff is essential.
Absorbing the demand for dementia care on medical wards diverts attention from other patient groups needing medical intervention. Consequently, the healthcare system experiences a cascade of operational inefficiencies. Delays in admissions for other patients may ensue, potentially complicating their conditions due to prolonged wait times. Such logistical bottlenecks place additional strain on the healthcare system, aggravating an already dire situation. Addressing these inefficiencies requires an immediate reassessment of current policies and a more strategic allocation of resources towards expanding adequate and secure psycho-geriatric facilities.
Comparing Dementia Care Approaches
Overseas Models of Care
Countries like Australia offer valuable insights into proactive strategies for dementia psychiatric care by adopting risk stratification systems with secure, specialized units for severe cases. These dedicated environments allow for focused, tailored interventions that mitigate risks associated with challenging behaviors while supporting holistic treatment plans. The presence of trained staff and purpose-built facilities facilitates a higher standard of care. This model reflects an understanding that the right setting and expertise are pivotal in managing dementia effectively, suggesting valuable lessons for New Zealand’s approach to this pressing issue.
Transposing these successful models to New Zealand requires a significant policy shift and an investment in specialized resources. Exploring the implementation of dedicated secure units would align the country’s healthcare standards with best practices observed internationally. Such a move necessitates collaboration between policymakers, healthcare providers, and medical staff to design environments conducive to comprehensive dementia care. Proactive planning fueled by insights from global counterparts can pave the way for enduring, effective solutions that accommodate the growing needs of older adults with psychiatric conditions.
Legal and Ethical Considerations
At the core of New Zealand’s dementia care challenge is the breach of patient rights, a legal and ethical issue that requires urgent rectification. Admitting dementia patients with acute psychiatric needs to general wards constitutes a violation of their right to receive adequate care. By not offering specialized environments, the healthcare system inadvertently compromises the safety and rights of both the affected patients and others sharing these wards. These breaches necessitate a reevaluation of current policies and underscore the importance of aligning care practices with national and international standards that prioritize patient safety and rights.
Resolving these issues is not only a matter of policy but also a responsibility involving ethical considerations of care delivery. Providing environments that respect the dignity and special needs of dementia patients reflects a commitment to ethical healthcare practices. It’s imperative to bridge the gap between existing protocols and optimal care conditions that support both patients’ rights and healthcare professionals’ ability to work safely and effectively. Reassessing care policies and creating infrastructures that respect legal and ethical standards are critical steps forward.
The Path to Adequate Dementia Care
Strategic Resource Allocation
To grapple with the growing demand for dementia psychiatric care, New Zealand must prioritize the allocation of resources towards expanding psycho-geriatric beds and facilities. The continuing reduction of beds, as evidenced by decisions in cities like Dunedin, indicates an alarming oversight in addressing this need. Financial limitations often cited as barriers to expanding resources should not outweigh the necessity for safe, effective care for dementia patients. A concerted effort involving governmental agencies, healthcare bodies, and funding institutions is essential to revisiting financial priorities and devising sustainable strategies to meet these critical needs.
Redirecting resources and attention to temporary solutions such as provisional secure accommodations can serve as interim measures while long-term strategies are implemented. Ensuring that current medical teams have access to support and additional training in managing dementia’s psychiatric components is also vital. While enduring solutions require time and planning, immediate actions can help mitigate current risks and lay down the groundwork for sustainable improvements. Reconfiguring existing resource allocations and exploring innovative care delivery models can significantly improve care outcomes across the board.
Collaborating for Change
Promoting change in New Zealand’s approach to dementia care hinges on collaborative efforts between various healthcare stakeholders, reflecting shared responsibility and commitment. Healthcare leaders, policymakers, and patient advocacy groups must work in tandem to address the deficiencies in current care models. By fostering conversations and collaborations across these domains, innovative solutions can be explored and implemented, leading to improved outcomes for all involved. Engaging experts from international medical circles can also provide valuable insights into crafting policies that are both compassionate and pragmatic.
Such collaboration is critical to driving policy changes that focus on enhancing care standards for dementia patients and ensuring that facilities are equipped to handle their specific needs. Meaningful change involves creating governance frameworks that facilitate effective communication and coordination across different healthcare tiers. Establishing continuous feedback mechanisms enables the identification and addressing of emerging challenges in a timely manner. The commitment to fostering dialogue and cooperation among healthcare sectors serves as the backbone for achieving lasting improvements in the care of dementia patients in New Zealand.
Steps Toward a Secure Future in Dementia Care
Dementia patients with Behavioral and Psychiatric Symptoms of Dementia (BPSD) encounter numerous obstacles when admitted to general medical wards lacking the proper facilities. Essential features like single rooms for patient safety and low-stimulus environments are often missing, exacerbating symptoms of distress. Exposure to constant lighting, noise, and improper interventions heightens anxiety, agitation, and perhaps aggression. Such care settings fall short of adhering to the New Zealand Code of Health and Disability Services Consumers’ Rights, which requires providing adequate care standards. Consequently, the lack of specialized care hinders effective management and treatment, detrimentally affecting their quality of life.
Furthermore, medical staff in these wards typically lack the specialized training necessary for managing dementia-related aggression and intricate behaviors, increasing the chance of adverse events. Misunderstanding or mishandling these symptoms can endanger both patients and staff. Without necessary resources or trained staff, healthcare settings may become risky, emphasizing the urgent need for dedicated psychiatric resources for dementia care.