I’m thrilled to sit down with Ivan Kairatov, a renowned biopharma expert with extensive experience in research and development, as well as a deep understanding of technological innovation in the industry. Today, we’re diving into a groundbreaking advancement in cancer treatment: the recent recommendation by the National Institute for Health and Care Excellence (NICE) for Keytruda, a therapy developed by MSD, to treat advanced endometrial cancer. Our conversation explores how this drug works, its significance for patients, the challenges of endometrial cancer, and what this milestone means for the future of oncology. Let’s get started.
Can you explain what Keytruda is and how it supports patients battling endometrial cancer?
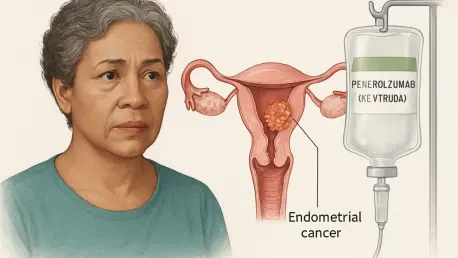
Keytruda, also known as pembrolizumab, is an immunotherapy drug that belongs to a class called anti-PD-1 therapies. Essentially, it boosts the body’s immune system to better detect and attack cancer cells by blocking a pathway that tumors often use to hide from immune detection. For endometrial cancer patients, this means it can help slow down or stop the growth of tumors. When combined with chemotherapy drugs like carboplatin and paclitaxel, it creates a powerful one-two punch—chemo directly attacks the cancer cells, while Keytruda enhances the immune response to clean up what’s left. This dual approach has shown really promising results for patients with advanced or recurrent disease.
Why is the NICE recommendation for Keytruda considered such a game-changer for patients in England and Wales?
This recommendation is huge because it means Keytruda will now be accessible through the National Health Service (NHS) for eligible patients with advanced or recurrent endometrial cancer. Before this, options were limited, especially for those with certain tumor types. What’s even more impactful is that it’s available immediately through the Cancer Drugs Fund, which speeds up access to innovative treatments while long-term funding decisions are finalized. For patients, this translates to hope—having a cutting-edge therapy at their fingertips without the burden of prohibitive costs or long delays can make all the difference in their fight against cancer.
Endometrial cancer affects thousands annually in the UK. Can you shed light on the major hurdles these patients face?
Absolutely. Endometrial cancer, the most common type of womb cancer, impacts over 9,700 people in the UK each year. One of the biggest challenges is late diagnosis. When caught early, survival rates are quite high, but if it’s found at stage 3 or 4, the five-year survival rate can drop to 50% or even less. Symptoms like abnormal bleeding can be mistaken for other conditions, delaying diagnosis. For advanced cases, the disease often spreads, making treatment more complex and less effective. Patients also face emotional and physical tolls—treatments can be grueling, and the uncertainty of recurrence looms large. That’s why new options like Keytruda are so critical.
Keytruda is recommended for both mismatch repair proficient and deficient tumors. Can you unpack these terms for us and explain their importance?
Sure, I’m happy to break this down. Mismatch repair proficient (pMMR) and mismatch repair deficient (dMMR) refer to how well a tumor’s DNA repair system functions. In dMMR tumors, this system is faulty, leading to more mutations and often a better response to immunotherapies like Keytruda because the immune system can more easily recognize these abnormal cells. pMMR tumors, on the other hand, have a working repair system, so they’re harder to target with immunotherapy and historically have fewer treatment options. The fact that Keytruda is effective for both types is a breakthrough—especially for pMMR patients, who’ve been underserved. It broadens the scope of who can benefit from this therapy significantly.
The KEYNOTE-868 trial had some exciting outcomes for Keytruda. Can you walk us through the most significant findings?
The KEYNOTE-868 trial was a pivotal study that really put Keytruda on the map for endometrial cancer. For patients with dMMR tumors, the results were striking—at a median follow-up of about 14 months, the group receiving Keytruda plus chemo hadn’t even reached a median progression-free survival, meaning many hadn’t seen their cancer worsen, compared to just 8.3 months for those on chemo alone. For pMMR tumors, the benefit was also clear—median progression-free survival was 13.1 months with Keytruda and chemo, versus 8.7 months with chemo only, at a follow-up of around 10 months. These numbers show that Keytruda can meaningfully extend the time patients live without their cancer progressing, which is a beacon of hope for better quality of life and outcomes.
From a biopharma perspective, what makes this NICE approval such a significant milestone?
From the industry standpoint, this approval is a major achievement. It validates years of research and investment into immunotherapy and shows that we’re moving toward more personalized, effective cancer care. For a company like MSD, it reinforces their commitment to tackling hard-to-treat cancers and positions Keytruda as a cornerstone in oncology. It’s not just about one drug—it’s about proving that immune-based therapies can address unmet needs across diverse patient groups. Plus, successes like this often pave the way for further innovation, encouraging exploration into other cancer types or combination therapies that could benefit even more patients down the line.
What is your forecast for the future of immunotherapy in cancer treatment, especially for diseases like endometrial cancer?
I’m incredibly optimistic about where immunotherapy is headed. We’re just scratching the surface of what drugs like Keytruda can do. For endometrial cancer, I expect we’ll see more tailored approaches—combining immunotherapies with targeted therapies or even novel agents to tackle resistance and improve outcomes further. Beyond that, advancements in biomarkers and diagnostics will help us identify which patients will respond best, minimizing trial and error. Industry-wide, there’s a push toward expanding these therapies to earlier stages of cancer and other tumor types. The next decade could transform cancer from a life-threatening diagnosis to a manageable condition for many, and I believe immunotherapy will be at the heart of that shift.