The market for gene therapies is predicted to surge from $9 billion in 2023 to $23.9 billion in 2028, according to MarketsandMarkets. With such rapid growth, it has become increasingly evident that having an effective analytical testing strategy is crucial for the successful development and production of viral vectors. Viral vectors are indispensable for the majority of gene therapies, and their quality directly impacts the therapeutic’s safety and efficacy. Michael Born, a manager with MilliporeSigma’s viral vector CDMO analytical development team, emphasizes the essential role of a well-crafted analytical testing strategy in meeting regulatory requirements and industry standards, ultimately ensuring the production of a high-quality, safe, and effective product.
An effective analytical testing strategy lays a solid foundation for a phase-appropriate development process. It helps in addressing complex challenges by ensuring compliance, scalability, and reproducibility of both the product and the process from an early stage. For those in the field, understanding and implementing a robust analytical testing strategy is imperative. Born provides a comprehensive playbook for designing an analytical testing strategy for viral vectors, which can be utilized whether working internally or with a Contract Development and Manufacturing Organization (CDMO) partner.
1. Comprehend Identification and Characterization Information
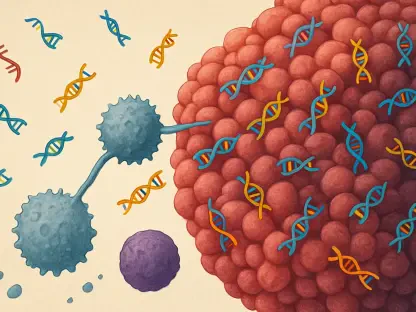
A crucial first step in designing an effective analytical testing strategy is understanding the identification and characterization data of viral vectors. Viral vectors consist of two main components: the vector itself, which encapsulates and delivers the nucleic material to the target, and the “cargo” or gene of interest (GOI). Identification and characterization tests are vital and can include structural elucidation, purity and impurity profiling, and advanced techniques like next-generation sequencing (NGS). NGS provides unparalleled insights into the genome, essential for confirming viral vector identities and detecting impurities. Ensuring thorough comprehension of these data assists in laying the groundwork for subsequent steps.
Characterization tests often include detailed profiling methods that go beyond basic identification. By employing next-generation sequencing, you gain a level of fidelity that ensures there are no mutations in the GOI, thus confirming the integrity of the vectors. This level of analysis is vital to ascertain the safety and effectiveness of the viral vectors. Additionally, this step helps in identifying any potential impurities that could compromise the quality of the final gene therapy product. Such meticulous attention to detail is fundamental in the early stages of viral vector development to meet stringent regulatory requirements.
2. Verify Your Preclinical Development Techniques
After establishing a clear understanding of identification and characterization data, it is essential to validate and qualify preclinical development methods. These methods should be tailored to meet appropriate phase and quality targets while considering future needs. Michael Born highlights the importance of proactive planning for commercial product requirements from the very start. This forward-thinking approach can involve using pharmacokinetics, pharmacodynamics, and toxicology evaluations supported by bioanalytical assays and mass spectrometry to characterize viral proteins and impurities at a molecular level.
Verification of preclinical development techniques involves a detailed evaluation to ensure that the methods used are both accurate and reliable. This stage is critical in streamlining the transition from preclinical to clinical phases, mitigating risks, and accelerating timelines. Bioanalytical assays play a vital role by offering insight into the biological activity and potential toxicity of the viral vectors. Mass spectrometry provides a molecular-level understanding, aiding in the accurate characterization of viral proteins and impurities. These combined techniques ensure that the therapeutic will be safe and effective as it progresses to the next phase of development.
3. Formulate Your Clinical Development Procedure
The clinical development phase is pivotal in advancing a therapeutic from preclinical to later stages, with a focus on bioavailability, bioequivalence, and immunogenicity testing. At this juncture, next-generation sequencing plays a significant role by offering in-depth analysis of virus-host interactions and potential immune responses. Leveraging these advanced techniques can help mitigate risks and expedite timelines, as emphasized by Michael Born. A well-formulated clinical development procedure ensures that the therapeutic complies with regulatory standards and meets the demands of clinical trials.
Formulating an effective clinical development process involves meticulous planning and execution. This phase addresses various challenges, including bioavailability, which assesses how well and how quickly the therapeutic reaches its target. Bioequivalence tests compare the new therapeutic to existing standards, ensuring consistency in therapeutic effects. Immunogenicity testing is crucial for evaluating the potential immune responses elicited by the viral vectors, which could affect both safety and efficacy. Utilizing the comprehensive analytical platforms offered by viral vector CDMOs can significantly enhance the quality and compliance of clinical trials.
4. Plan Your Clinical Manufacturing Workflow
The clinical manufacturing process should be meticulously planned from the earliest stages to meet the demands of the patient population. A consistent product is achieved through well-designed process development, which is crucial long before the actual manufacturing begins, as noted by Michael Born. Designing this process involves implementing in-process controls, impurity profiling, and leveraging techniques like mass photometry for high-throughput analysis and optimization of purification processes.
A robust clinical manufacturing workflow aims to ensure that each batch of the therapeutic is consistent in quality and efficacy. In-process controls are employed to monitor critical parameters during manufacturing, guaranteeing that the final product adheres to specified standards. Impurity profiling identifies and quantifies potential contaminants, ensuring the safety of the therapeutic. Mass photometry is utilized for rapid and detailed analysis, optimizing the purification processes to achieve high levels of purity and concentration. These steps are essential in scaling up production while maintaining the therapeutic’s integrity and effectiveness.
5. Emphasize Quality Control Records
Maintaining impeccable quality control records is imperative for both regulatory approval and the ongoing success of the therapeutic. Regulatory authorities demand comprehensive data packages prior to granting approvals, which include batch release tests and ongoing quality control evaluations for identity, strength, purity, and quality attributes. Techniques such as next-generation sequencing, mass photometry, and mass spectrometry are employed to ensure consistency and compliance, as highlighted by Michael Born.
Quality control records serve as comprehensive documentation of every aspect of the manufacturing process, from raw materials to final product release. These records are scrutinized by regulatory authorities to ensure that the therapeutic meets all safety and efficacy standards. Next-generation sequencing provides a detailed genetic profile, confirming the identity and integrity of the viral vectors. Mass photometry and mass spectrometry offer precise measurements of purity and impurity levels, ensuring that each batch of the therapeutic is consistent in quality. Maintaining detailed and accurate quality control records is essential for the successful approval and ongoing production of viral vector-based gene therapies.
6. Evaluate Formulation and Stability
The final formulation of the gene therapy product must ensure stability under various environmental and physical stressors. According to Michael Born, formulation is critically important for buffering the drug from these stressors and maintaining its stability. This step includes stability, solubility, and compatibility tests with buffer excipients, using techniques like mass photometry for rapid, detailed analysis of viral vector subpopulations. Optimizing manufacturing conditions based on these evaluations is crucial for extending the shelf life of the drug.
Evaluating formulation and stability involves comprehensive testing to ensure that the final product remains effective and stable throughout its intended shelf life. Stability tests assess how the therapeutic responds to different environmental conditions, such as temperature fluctuations and light exposure. Solubility tests determine the optimal conditions for the therapeutic to remain in solution, enhancing its efficacy. Compatibility tests ensure that the buffer excipients used do not negatively interact with the viral vectors. Mass photometry provides a detailed analysis of viral vector subpopulations, ensuring consistency and stability. These evaluations are crucial in delivering a high-quality therapeutic that maintains its effectiveness over time.
7. Maintain Post-Market Monitoring
Even after a therapeutic reaches the market, meticulous post-marketing surveillance remains crucial. This phase involves monitoring batch-to-batch consistency and stability to identify any potential problems that could appear after commercialization. Tools like next-generation sequencing help in spotting unwanted agents, while mass spectrometry ensures consistent product quality. Continuous surveillance is vital for detecting and addressing any deviations from set quality standards, thereby maintaining the safety and efficacy of the therapeutic.
Post-market monitoring forms an essential part of the overall analytical testing strategy, ensuring the therapeutic complies with regulatory standards and retains its effectiveness. Monitoring batch-to-batch consistency ensures uniform quality across all units produced. Stability tests confirm that the product sustains its intended properties over time. The detection of unwanted agents, which could compromise safety, is facilitated by next-generation sequencing. Mass spectrometry continuously verifies product quality, ensuring the therapeutic remains safe and effective for patient use.
In summary, the production of safe, effective, high-quality viral vector therapeutics hinges on a well-structured analytical testing strategy. A phase-appropriate process allows innovators to speed up timelines, minimize risks, and bring crucial therapeutics to patients more efficiently. MilliporeSigma, with its vast experience in manufacturing viral vectors, partners with gene therapy innovators to strengthen their analytical testing strategies, supporting them from development through to commercialization.