Today we’re joined by Ivan Kairatov, a biopharma expert with a deep understanding of the technological innovations driving the industry, particularly in oncology. His work at the intersection of research and development gives him a unique perspective on the recent FDA clearance for PharmaResearch’s PRD-101, a novel nano-based cancer drug. This development represents a significant step for a company pivoting from regenerative medicine into the competitive oncology space, and Ivan is here to help us unpack what it all means.
We’ll be exploring the science behind PharmaResearch’s proprietary DOT platform and how it aims to solve long-standing toxicity issues with solid tumor treatments. Ivan will also provide his insights into the upcoming Phase I clinical trial, discussing the critical metrics for success and the potential challenges ahead. We’ll look at how this new class of nano-formulated drugs could fundamentally alter the patient experience and treatment outcomes, and examine the strategic collaborations that are paving the way for this technology.
PharmaResearch’s DOT platform uses nucleotide fragments to improve drug loading and pharmacokinetics. Could you explain the mechanism behind this technology and how it specifically aims to overcome the toxicity limitations seen in conventional solid tumor therapies? Please provide some step-by-step details.
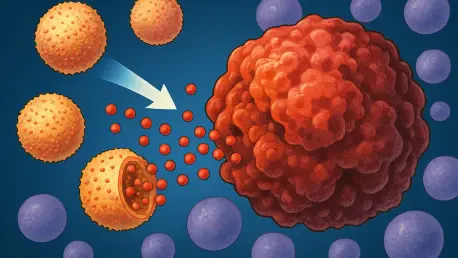
Of course. The DOT platform is a fascinating approach because it’s not just a vehicle; it’s an integrated system built from biological components. The process starts with DNA, which is broken down into optimized nucleotide fragments. Think of these fragments as custom-designed, intelligent building blocks. These blocks are then used to construct the nanoparticle, which serves as the delivery system. Because they are derived from DNA, these nanoparticles have an inherent compatibility that allows for much more efficient drug loading compared to many synthetic polymers. This improved loading means more therapeutic payload gets packed into each particle. The second key step is how it behaves in the body. The nanoparticle is engineered to have superior pharmacokinetic properties, meaning it can circulate longer and more effectively reach the tumor microenvironment while avoiding rapid clearance by the body. This targeted approach is how it tackles toxicity; by concentrating the anticancer agent at the tumor site, you drastically reduce its exposure to healthy tissues, which is the root cause of the debilitating side effects we see with so many conventional chemotherapies.
The upcoming Phase I trial for PRD-101 will assess safety and pharmacokinetics in patients with advanced solid tumors. Beyond standard safety metrics, what specific endpoints or biomarkers will be most critical for establishing a viable dose, and what operational challenges do you anticipate?
In a first-in-human trial like this, safety is paramount, but the real art is in gathering the data that will guide the entire future of the drug. Beyond just recording adverse events, the most critical pharmacokinetic data will involve intensive blood sampling to map precisely how PRD-101 is absorbed, distributed, metabolized, and excreted. We need to see if the nanoparticle is behaving as designed—is it staying in circulation long enough? Is it clearing the body in a predictable way? This data is what directly informs the dose-escalation decisions and helps us find that sweet spot: the maximum tolerated dose that still shows potential for efficacy. While this is primarily a safety study, investigators will undoubtedly be looking for early, exploratory biomarkers of anti-tumor activity, such as changes in tumor markers or even preliminary imaging scans, to get a hint that the drug is hitting its target. Operationally, coordinating a trial across up to seven US sites with approximately 90 patients presents a significant logistical challenge. A novel nano-formulated agent requires specialized handling, storage, and infusion protocols. Ensuring absolute consistency across all clinical sites is a massive undertaking, as any variability could compromise the integrity of the safety and pharmacokinetic data, which is the entire foundation for moving forward.
Many oncology drugs face dose limitations due to severe side effects. How might a nano-formulated agent like PRD-101 change the treatment paradigm for patients with advanced solid tumors? Please walk us through the potential differences in patient experience and clinical outcomes.
This is really the heart of why this technology matters so much. For a patient with an advanced solid tumor, the treatment journey is often a brutal trade-off between fighting the cancer and enduring the toxicity of the cure. Conventional therapies can feel like a poison, causing debilitating nausea, fatigue, and organ damage that forces physicians to limit the dose, often below what might be most effective. A nano-formulated agent like PRD-101 could completely rewrite that experience. By improving the therapeutic index—that is, maximizing the drug’s effect on the tumor while minimizing its effect on the body—we could potentially administer more effective doses with fewer side effects. Imagine a patient who can continue treatment for longer, without the constant interruptions needed to recover from toxicity. This could mean a more sustained attack on the tumor, potentially leading to better clinical outcomes and a dramatically improved quality of life, allowing them to feel more like themselves during a very difficult fight.
PharmaResearch is leveraging its DOT platform to pivot from regenerative medicine to oncology, collaborating with academic centers. How does this strategic shift and these partnerships help de-risk a novel platform technology? Could you share some insights on the steps involved in this process?
Pivoting a core technology into a new, highly competitive field like oncology is a high-risk, high-reward maneuver. PharmaResearch’s strategy here is very shrewd. First, by applying their established DOT platform to a new therapeutic area, they aren’t starting from scratch; they are building on a technology they already understand deeply. The primary de-risking step comes from their collaborations. Partnering with a prestigious institution like the University of California, Irvine, and leveraging the resources of the National Cancer Institute’s Nanotechnology Characterization Laboratory is crucial. These academic and governmental partners provide immense validation. They bring world-class oncology expertise, sophisticated analytical capabilities, and an unbiased, rigorous scientific lens to the preclinical development. This process involves sharing data, co-designing experiments, and having external experts stress-test the technology, which helps identify potential weaknesses long before the immense expense of a clinical trial. This external validation is not just scientifically valuable; it’s a powerful signal to regulators and future investors that the platform is robust and has been vetted by leaders in the field.
What is your forecast for the role of nucleotide-based nanoparticle therapeutics in oncology over the next decade?
I believe we are standing at the threshold of a new era for these types of therapeutics. For years, the challenge in oncology hasn’t just been finding potent drugs, but getting them to the right place without devastating the patient. Nucleotide-based nanoparticles, like the DOT platform, represent a significant leap in solving that delivery problem. Over the next decade, I forecast that we’ll see this technology mature from early-phase trials into a validated class of medicines. We will likely see them used not just to deliver single agents more safely, but as platforms for complex combination therapies, carrying multiple payloads to attack cancer from different angles simultaneously. As our understanding of tumor biology deepens, the precision and versatility of these nucleotide-based systems will become indispensable, potentially unlocking the full potential of powerful drugs that were previously considered too toxic to use. They won’t just be an incremental improvement; they will become a foundational tool for building the next generation of smarter, kinder cancer treatments.