Recent studies have unraveled groundbreaking findings around stem cell involvement in the olfactory system, revealing promising avenues to restore the sense of smell. Despite the common perception that neurons, once lost, cannot regenerate, olfactory neurons challenge this understanding as they possess a lifelong ability to regenerate. Researchers at Tufts University School of Medicine and the Graduate School of Biomedical Sciences have delved deep into the mysteries of olfactory neurogenesis. They’ve unveiled the mechanisms by which these neurons replenish in the nasal cavity and identified specific stem cells responsible for this extraordinary regeneration. By understanding these biological processes, new therapeutic solutions could be developed for those suffering from anosmia—a condition characterized by the loss of smell either post-viral infection, such as COVID-19, or due to aging. This research has employed innovative models and has exposed new potential pathways for drug development, holding promise to effectively combat olfactory dysfunctions.
Unlocking Olfactory Neurogenesis
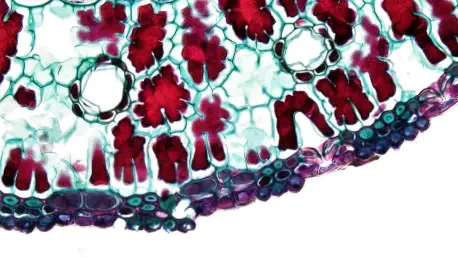
Olfactory neurons are unique among sensory neurons due to their capability to regenerate throughout an individual’s life. This regenerative prowess contrasts with other parts of the nervous system, like the central nervous system, which lacks such an ability. The key players in this regenerative process appear to be specific types of stem cells in the nasal cavity. Two types of stem cells, horizontal basal cells (HBCs) and globose basal cells (GBCs), have been identified as integral to olfactory neuron regeneration. HBCs, previously thought to be largely dormant, have now been shown to play an active role in neurogenesis and olfactory tissue repair. Marked by the protein KRT5, HBCs are pivotal in generating new neurons, aiding in sustained olfactory function. The discovery of their active involvement underlines the incredible adaptability and resilience of the olfactory system, significantly advancing our understanding of sensory neurogenesis.
Aging and viral infections have been found to seriously impact the population and function of these basal cells. As individuals age, there is a noted decline in GBC populations, correlating directly with reduced neuron production. This contributes to the diminished sense of smell commonly associated with aging. Additionally, viral infections like COVID-19 can disrupt normal neurogenesis, leading to conditions such as post-viral anosmia. Understanding the dynamics of these stem cells offers insights into potential therapeutic targets, whereby drugs or treatments can be developed to promote the regeneration of olfactory neurons and, consequently, restore the sense of smell. By identifying the mechanisms through which these cells contribute to neurogenesis, researchers can devise targeted interventions to mitigate the effects of aging and viral infections on olfactory function.
Innovations in Modeling and Therapeutics
To effectively study the intricacies of olfactory neuron formation, researchers have developed a pioneering 3D mouse olfactory tissue organoid model. This innovative model provides an accessible, low-cost platform to analyze the processes governing olfactory neurogenesis. By simulating the in vivo conditions of the nasal environment, this model allows scientists to observe neuron production and understand declines associated with disease and aging. The development of such organoid models heralds a new age in preclinical research, offering more efficient and less costly alternatives to traditional animal models and human cell cultures. These models democratize research efforts, enabling labs with limited resources to contribute to the broader scientific understanding of olfactory regeneration.
The quest now is to translate these findings into human organoid models, which could facilitate drug screening and potential therapies for anosmia. Human organoid development presents unique challenges, particularly in isolating pure olfactory tissue from humans. Despite these challenges, advancements in this area could open doors to groundbreaking treatments. By focusing on stem cell function and olfactory regeneration, researchers aim to create targeted therapies that can address not only anosmia but also other sensory deficits and related conditions. The ultimate goal is to harness these findings to develop pharmaceuticals and interventions that can promote neurogenesis and restore the full range of olfactory abilities.
Future Directions and Implications
Recent studies have brought groundbreaking insights into the role of stem cells in the olfactory system, opening up promising possibilities for restoring the sense of smell. Contrary to the common belief that neurons cannot regenerate once lost, olfactory neurons defy this notion as they can regenerate throughout a person’s life. Researchers from Tufts University School of Medicine and the Graduate School of Biomedical Sciences have explored the complexities of olfactory neurogenesis, discovering the mechanisms that enable these neurons to regenerate in the nasal cavity. They have identified specific stem cells responsible for this remarkable regenerative ability. With a better understanding of these biological processes, new therapies could be developed for individuals suffering from anosmia—a condition marked by loss of smell due to factors like viral infections such as COVID-19 or aging. This research has utilized innovative models and revealed new potential pathways for drug development, offering hope to effectively address olfactory dysfunctions.