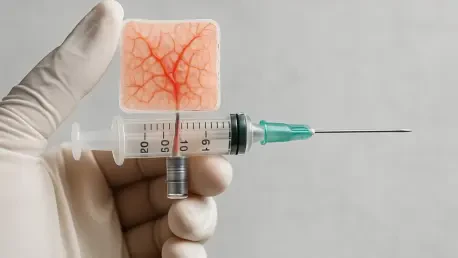
Imagine a world where the devastating impact of severe burns and deep wounds can be reversed with a tool as simple as a syringe, delivering regenerated skin that mirrors the real thing in both appearance and function. A pioneering advancement from researchers at Linköping University in Sweden is turning this vision into a tangible reality with a technology metaphorically termed “skin in a syringe.” This innovative approach harnesses a bioengineered gel infused with living cells to create skin transplants that promise to redefine treatment for major injuries. Unlike conventional grafts that often result in scarring and incomplete recovery, this method focuses on restoring the dermis—the deeper, vital layer of skin responsible for elasticity and critical structures like blood vessels. The potential to heal with precision and personalization could offer new hope to burn victims facing life-altering challenges, marking a significant leap forward in regenerative medicine and wound care.
Overcoming the Limits of Traditional Skin Grafts
The shortcomings of traditional skin grafting techniques have long posed a significant barrier to effective healing for burn victims and those with severe wounds. Most grafts primarily address the epidermis, the outermost layer of skin, while largely ignoring the dermis beneath it. The dermis plays an indispensable role in providing strength, flexibility, and the capacity to heal without debilitating scarring. When it is not adequately restored, patients often endure long-term issues such as restricted movement, chronic discomfort, and an increased risk of infection. This gap in treatment has driven the need for a solution that can regenerate the dermis in a way that mirrors natural skin structure, addressing both functional and aesthetic outcomes. The challenge lies in the complexity of this deeper layer, which contains intricate networks of blood vessels, nerves, and hair follicles, making it a difficult target for replication using existing medical approaches.
A novel strategy emerging from recent research offers a promising alternative by leveraging the body’s own healing capabilities rather than attempting to fully recreate the dermis in a lab setting. By embedding fibroblasts—key connective tissue cells—within a supportive gel, the technology provides essential building blocks for dermal regeneration. Applied directly to the wound via syringe or 3D printing, this material encourages the natural formation of a functional dermis over time. This approach sidesteps the limitations of traditional methods by focusing on integration with the patient’s biology, potentially reducing scarring and improving recovery outcomes. Early evidence suggests that such a method could transform how severe skin injuries are treated, offering a more holistic restoration of skin integrity that prioritizes long-term functionality over temporary coverage.
Innovations in Bioengineered Materials
At the core of this transformative technology is a meticulously designed gel that replicates the natural environment of human skin, providing an ideal setting for cellular growth and healing. Composed of gelatin beads that emulate collagen—a fundamental component of skin structure—and hyaluronic acid, a substance naturally present in the body, the gel ensures biocompatibility while fostering tissue regeneration. The gelatin acts as a scaffold, supporting the growth of fibroblasts, while hyaluronic acid enhances the material’s suitability for medical application by aiding in moisture retention and tissue repair. This carefully balanced combination not only sustains living cells but also adapts to the practical demands of clinical use, making it a versatile tool for addressing complex wounds with precision and care.
What sets this gel apart is its remarkable ability to transition between states, adapting to the needs of application and integration. Under slight pressure, such as when dispensed through a syringe or a 3D printer, it becomes a liquid, allowing for accurate placement directly onto a wound site. Once in contact with the skin, it reverts to a stable, gel-like form, securing the embedded cells in place to initiate the healing process. This dynamic property facilitates customized application, enabling medical professionals to tailor the treatment to the specific shape and depth of an injury. Such adaptability marks a significant advancement in materials science, bridging the gap between laboratory innovation and real-world medical needs, and paving the way for more effective and less invasive wound care solutions that could redefine standards in regenerative medicine.
Addressing Vascular Challenges in Tissue Engineering
One of the most persistent obstacles in tissue engineering is ensuring that newly created tissues receive adequate oxygen and nutrients through a network of blood vessels, a process known as vascularization. Without this critical supply, engineered skin or larger tissue constructs risk cell death in their central regions, severely limiting their size and viability for clinical use. This challenge has hindered progress in developing comprehensive solutions for burn treatment and beyond, as the absence of a vascular system prevents full integration with the body’s natural processes. Researchers have recognized that solving this issue is pivotal not only for skin regeneration but also for broader applications in creating functional organ-like structures for medical research or therapeutic purposes, highlighting the urgency of innovative approaches.
In tandem with the development of the bioengineered gel, the team at Linköping University is exploring a complementary innovation involving hydrogel threads—tiny, water-based structures capable of forming perfusable channels. These miniature tubes, composed of materials that are predominantly water, demonstrate impressive elasticity and the potential to support blood vessel growth within engineered tissues. Initial experiments in animal models have shown encouraging results, with fibroblasts in the gel not only surviving but also contributing to the production of dermal materials and the formation of blood vessels. This dual focus on skin regeneration and vascularization suggests a future where such technology could extend its impact, potentially influencing fields like organoid development and offering new avenues for treating a wide range of conditions with greater efficacy.
Future Horizons in Regenerative Medicine
Looking ahead, the implications of this technology extend far beyond the immediate treatment of burns and wounds, pointing to a transformative shift in how regenerative medicine is approached. The ability to 3D print a gel infused with living cells introduces a level of customization that could tailor treatments to the unique needs of each patient, enhancing outcomes through precision. As the gel supports natural dermal regeneration, it also opens possibilities for reducing the physical and emotional toll of scarring, giving patients a chance at recovery that more closely resembles their pre-injury state. Continued research and clinical trials over the coming years, starting from now through the next decade, will be crucial in determining how effectively this method can transition from experimental models to widespread medical practice, potentially setting a new benchmark for personalized care.
Reflecting on the progress made, the journey of this bioengineered solution showcased a remarkable blend of materials science and medical innovation when early tests in mice revealed the survival of cells and the emergence of blood vessel networks. These initial successes underscored the potential for the gel to act as a catalyst for natural healing, a concept that captivated the scientific community. As researchers collaborated across disciplines, their efforts illuminated a path toward addressing not just skin injuries but also broader challenges in tissue engineering. Moving forward, the focus should shift to scaling these findings into human applications, refining the technology for safety and efficacy, and exploring its adaptability to other medical fields. This pioneering work lays a foundation that, with sustained investment and exploration, could reshape the landscape of healing, offering solutions that were once thought impossible.