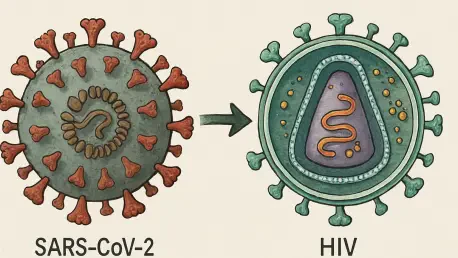
In a remarkable and deeply concerning case that has gripped the attention of medical researchers and public health experts alike, a 41-year-old man with advanced, untreated HIV carried a SARS-CoV-2 infection for an unprecedented 776 days. This extraordinary duration, detailed in a study recently published in The Lancet Microbe, offers a rare and unsettling window into the virus’s ability to adapt and evolve within a single human host. Conducted by scientists from Boston University and the Harvard T.H. Chan School of Public Health, the research not only chronicles the patient’s prolonged battle with COVID-19 but also raises critical alarms about the potential for immunocompromised individuals to become unintended incubators for new viral variants. The implications stretch far beyond this individual tragedy, pointing to systemic vulnerabilities in global health frameworks. With millions worldwide lacking access to essential treatments for conditions like HIV, the risk of similar long-term infections looms large, demanding urgent attention and action from the scientific and policy communities.
Viral Evolution in a Unique Host
A Glimpse into Prolonged Viral Adaptation
The sheer length of the SARS-CoV-2 infection in this patient—spanning 776 days from initial symptoms in 2020 to his passing in 2022—stands as a stark anomaly in medical records. Genomic sequencing of multiple samples taken over this period revealed a staggering array of changes within the virus, which belonged to an early B.1 lineage. Astonishingly, mutations in the spike protein mirrored defining traits of the Omicron variant, emerging in the patient before Omicron swept across the globe. This finding suggests that persistent infections can independently foster significant viral adaptations, even without exposure to circulating strains. The patient’s body essentially became a secluded environment where the virus could experiment with genetic alterations, unhindered by typical immune defenses. Such a scenario underscores the unpredictable nature of viral evolution in unique hosts and highlights the importance of studying these rare cases to better anticipate future viral behavior.
The Role of a Compromised Immune System
The patient’s severely weakened immune system, a direct result of untreated HIV with an extremely low CD4+ count, provided fertile ground for the virus to thrive unchecked. Unlike typical infections where immune responses eventually clear or suppress the pathogen, this case allowed SARS-CoV-2 to replicate continuously for over two years. Analysis showed the coexistence of multiple viral subpopulations within the host, each evolving along distinct paths. The high ratio of non-synonymous to synonymous mutations pointed to selective pressures, likely driven by host-specific factors, that favored adaptations enhancing persistence. This environment of minimal immune resistance created a unique dynamic where the virus could refine its genetic makeup over time. Understanding these mechanisms is crucial, as they reveal how immunosuppression can transform a human body into a long-term reservoir for viral experimentation, potentially leading to significant shifts in viral characteristics.
Public Health Risks and Systemic Challenges
Assessing the Threat of Transmission
Despite the patient’s consistently high viral loads over the 776-day infection, detailed phylogenetic analysis found no evidence of onward transmission in global SARS-CoV-2 databases. The virus formed a distinct monophyletic clade, with several mutations being rare or entirely unique, suggesting that adaptations for persistence within this host may have reduced its ability to spread to others. However, this lack of detected spread could also be attributed to the patient’s rural location in South Carolina, where public health infrastructure and surveillance systems, such as wastewater monitoring, are often limited. The possibility of short, undetected transmission chains cannot be ruled out, raising concerns about gaps in monitoring capabilities in less-resourced areas. This situation highlights a critical blind spot in current systems, where localized outbreaks or variant emergence might go unnoticed until they escalate into broader threats, necessitating more robust and widespread surveillance efforts.
Linking Individual Cases to Global Vulnerabilities
The broader implications of this case extend far beyond a single patient, pointing to systemic issues that affect millions globally. With over one-third of people with HIV in the U.S. not virally suppressed and nearly 10 million worldwide lacking access to antiretroviral therapy (ART), the conditions for persistent SARS-CoV-2 infections are disturbingly common. Such long-term infections in immunocompromised individuals could serve as potential breeding grounds for new variants, especially in regions with limited healthcare access. This case exemplifies how individual health crises are intertwined with global health security, as untreated chronic conditions like HIV amplify the risk of viral evolution with far-reaching consequences. Addressing these vulnerabilities requires not only improved access to treatments but also integrated care models that tackle both HIV and COVID-19 simultaneously. Without such interventions, the specter of variant emergence remains a persistent threat to pandemic preparedness.
A Call for Enhanced Strategies and Equity
Reflecting on this alarming case, it becomes evident that the intersection of personal health challenges and global pandemics demands a coordinated and equitable response. The insights gained from the 776-day infection underscore the urgent need for expanded access to ART for HIV patients, ensuring that immunosuppression does not become a gateway for prolonged viral persistence. Routine genomic surveillance of high-risk populations is also deemed essential to detect unusual viral evolution early and prevent potential outbreaks. Moreover, integrating care for coexisting conditions like HIV and COVID-19 emerges as a critical step to mitigate risks. Bridging gaps in healthcare access, particularly in underserved regions, stands out as a necessary measure to protect both individual and community health. These actions, taken in response to the lessons learned, aim to fortify global health systems against the unpredictable nature of viral threats, ensuring that such extraordinary cases do not herald the rise of new, dangerous variants.