The global healthcare community has long grappled with the persistent challenge of chronic wounds, debilitating injuries that fail to heal in a timely and orderly fashion, often leading to severe complications for patients, particularly those with conditions like diabetes. Traditional wound care has primarily relied on passive dressings that serve as protective barriers, shielding the injury from infection but contributing little to the underlying biological healing process. However, a significant paradigm shift is emerging from a research team at the University of Nizwa in Oman, where scientists are pioneering a groundbreaking treatment that transforms the very concept of a wound dressing. By leveraging the precision of 3D bioprinting, they are creating an advanced, active dressing designed not merely to cover a wound, but to intelligently and dynamically participate in its regeneration. This innovative approach promises to foster an ideal healing environment, actively stimulating tissue repair and modulating the body’s inflammatory response to accelerate recovery and improve patient outcomes.
A New Paradigm in Wound Care
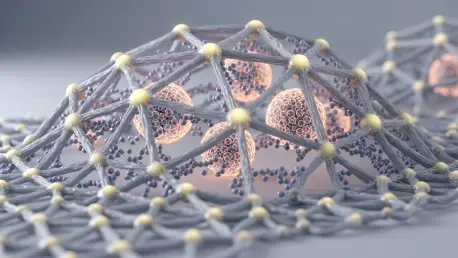
The core innovation behind this advanced treatment lies in its departure from conventional passive methods, introducing a dressing that functions as an active biological agent. The team, based at the Laboratory for Stem Cell Research and Regenerative Medicine, employs 3D bioprinting to construct a sophisticated scaffold using carboxymethyl chitosan, a biocompatible and biodegradable material known for its ability to support tissue regrowth. This structural framework is then infused with tacrolimus, a potent immunosuppressive drug. The resulting dressing serves a critical dual purpose: while the chitosan scaffold provides the physical structure necessary for new cells to populate and rebuild damaged tissue, the tacrolimus is released in a controlled, sustained manner directly at the wound site. This targeted drug delivery actively regulates inflammatory responses, which are often a key reason why chronic wounds fail to heal properly. By creating an environment that simultaneously encourages regeneration and reduces harmful inflammation, the dressing becomes an integral part of the healing cascade itself.
This pioneering work, led by Dr. Sulaiman bin Ali al Hashmi, has already garnered significant acclaim within the scientific community, underscoring its potential to revolutionize wound management. The project’s profound impact was formally recognized when it was awarded first place at the 12th National Research Award in 2025, a prestigious honor that highlights its significant contributions to the field of regenerative medicine and its promising path toward clinical application. This award serves as a powerful validation of the team’s novel approach, which aligns with the foremost goals of modern therapeutic research: to develop treatments that work in concert with the body’s innate healing capabilities. By engineering a solution that actively stimulates and guides the regenerative process, the researchers are not just creating a better bandage but are establishing a new benchmark for what is possible in the treatment of hard-to-heal injuries, offering new hope to a growing patient population worldwide.
From Laboratory to Clinical Application
While the 3D-bioprinted dressing holds immense promise, it currently remains in the experimental phase and has not yet been approved for use in human patients. The research team has been meticulously evaluating its efficacy and safety through a series of rigorous laboratory tests and comprehensive animal studies. The initial findings from these preclinical trials have been exceptionally encouraging, providing strong evidence to support the treatment’s underlying scientific principles. In these studies, wounds treated with the active dressing demonstrated a markedly accelerated healing rate compared to those managed with conventional methods. Furthermore, researchers observed a significant reduction in key inflammatory markers at the injury site, confirming the effectiveness of the controlled-release tacrolimus in modulating the immune response. These positive results are a critical step forward, building a solid foundation of data that will be essential for advancing the technology toward future clinical trials and eventual patient use.
The journey from a conceptual breakthrough to a viable medical product is rarely without its obstacles, and this project was no exception. Dr. Hashmi and his team acknowledged encountering several significant technical hurdles during the development process. One of the primary challenges involved formulating a bioprintable material that possessed the precise viscosity, biocompatibility, and structural integrity required for both the 3D printing process and effective wound healing. Additionally, translating this advanced laboratory research into a scalable, clinically applicable treatment was hampered by limitations in the available high-tech infrastructure. However, these difficulties did not derail the project; instead, they served to strengthen the team’s resolve and foster a more robust collaborative environment. Overcoming these challenges required ingenuity and perseverance, ultimately enriching the research process and leading to a more refined and resilient final product, better prepared for the rigorous demands of real-world medical application.
The Path Forward for Regenerative Healing
The culmination of this intensive research and development phase established a clear and ambitious trajectory for the future. The researchers planned to continue their dedicated work in the broader fields of stem cell research and regenerative medicine, using the insights gained from this project as a springboard for further innovation. Their primary objective was to meticulously refine the treatment model, optimizing the material composition, drug-release kinetics, and 3D-printing protocols to maximize healing efficacy and ensure patient safety. The ultimate goal of the team was always centered on the successful translation of their scientific findings from the laboratory bench to the patient’s bedside. This commitment was driven by the profound potential to dramatically improve the quality of life for individuals suffering from the debilitating effects of chronic wounds, transforming a novel scientific concept into a practical and life-changing therapeutic reality.