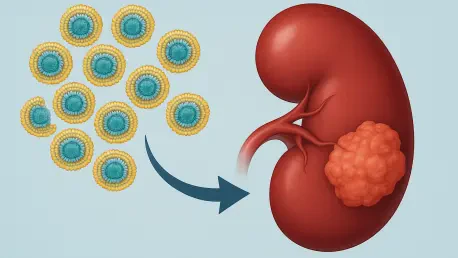
Lipid reprogramming has emerged as a critical frontier in understanding and treating clear cell renal cell carcinoma (ccRCC), the predominant subtype of kidney cancer that accounts for a significant portion of cases worldwide. This metabolic transformation, where tumor cells drastically alter how they handle lipids, serves as both a driver of cancer progression and a potential Achilles’ heel for therapeutic intervention. In ccRCC, cancer cells hoard fats through increased uptake and synthesis while curbing breakdown processes, creating a lipid-rich environment that fuels rapid growth and resilience. Yet, this very adaptation opens doors to innovative treatments by exposing vulnerabilities, particularly through mechanisms like ferroptosis, an iron-dependent form of cell death tied to lipid peroxidation. The challenge lies in exploiting these metabolic quirks without harming healthy tissues, a puzzle that researchers are racing to solve with targeted therapies and combination strategies. This article navigates the complex landscape of lipid metabolism in ccRCC, shedding light on how these cellular changes underpin tumor behavior and inspire cutting-edge approaches to therapy. From disrupting lipid stockpiles to inducing lethal oxidative stress, the potential to transform patient outcomes is tangible. As science unravels the intricate dance between metabolism and malignancy, a new era of personalized medicine for kidney cancer looms on the horizon, promising hope for those grappling with this aggressive disease.
Unraveling the Metabolic Shift in Renal Cancer
Lipid reprogramming stands as a defining characteristic of clear cell renal cell carcinoma, fundamentally reshaping how tumor cells manage fats to sustain their aggressive growth. This metabolic overhaul is largely orchestrated by the loss of the Von Hippel-Lindau (VHL) tumor suppressor gene, a genetic alteration common in ccRCC that triggers a cascade of changes. The resulting stabilization of hypoxia-inducible factors, specifically HIF-1α and HIF-2α, drives the expression of proteins that enhance lipid uptake and storage. These proteins act as conduits, pulling in fatty acids and cholesterol from the surrounding environment to build a stockpile that supports tumor expansion. This process isn’t merely a byproduct of cancer—it’s a deliberate adaptation that equips cells with the resources needed for rapid proliferation and survival under stress. Understanding this shift is pivotal, as it highlights why ccRCC tumors often appear lipid-laden under microscopic examination, a feature tied to their malignancy.
Beyond uptake, ccRCC cells ramp up internal lipid production through a process known as de novo synthesis, ensuring a steady supply even when external sources dwindle. Enzymes such as ATP-citrate lyase (ACLY) and fatty acid synthase (FAS) are key players, working in overdrive to churn out fatty acids from basic building blocks. Meanwhile, the breakdown of lipids through pathways like fatty acid β-oxidation is stifled, with enzymes such as carnitine palmitoyltransferase 1A (CPT1A) being suppressed. This imbalance results in the accumulation of lipid droplets, a hallmark of ccRCC that not only fuels growth but also correlates with poorer patient outcomes. The metabolic rewiring, driven by the VHL-HIF axis, positions lipid handling as a central pillar of tumor biology, offering a clear target for disrupting cancer progression.
The Dual Nature of Lipid Accumulation and Cell Death
In clear cell renal cell carcinoma, the massive buildup of lipids does more than just support tumor growth—it creates a unique susceptibility to a form of programmed cell death known as ferroptosis. This iron-dependent mechanism relies on the accumulation of toxic lipid peroxides, which can rupture cell membranes if not neutralized. The lipid-rich state of ccRCC, particularly the abundance of polyunsaturated fatty acids (PUFAs), makes these cells inherently prone to such oxidative damage. Enzymes like acyl-CoA synthetase long-chain family member 4 (ACSL4) amplify this risk by embedding PUFAs into membrane structures, setting the stage for potential cellular destruction. This vulnerability represents a double-edged sword: while it poses a threat to the tumor, it also offers a therapeutic window to exploit through carefully designed interventions aimed at triggering ferroptosis.
However, ccRCC cells are not passive victims of their lipid burden; they deploy sophisticated defenses to resist ferroptosis and maintain survival. The cystine/glutamate antiporter system xc⁻ is often upregulated, increasing the uptake of cystine to produce glutathione (GSH), a crucial antioxidant that counters lipid peroxidation. Additionally, glutathione peroxidase 4 (GPX4) plays a protective role by using GSH to detoxify peroxides, while ferroptosis suppressor protein 1 (FSP1) provides a secondary shield through coenzyme Q10 reduction. These mechanisms, bolstered by environmental and epigenetic factors, create a robust barrier against oxidative stress. The tumor’s ability to store PUFAs in lipid droplets as neutral fats further mitigates risk, reducing their availability for peroxidation. This intricate balance between susceptibility and resistance underscores the challenge of harnessing ferroptosis for therapy.
Disrupting Lipid Metabolism as a Treatment Strategy
Targeting lipid metabolism in clear cell renal cell carcinoma offers a promising pathway to hinder tumor growth by severing a critical lifeline that cancer cells rely on for survival. One focal point is the inhibition of upstream regulators like HIF-2α, which drives much of the lipid reprogramming in ccRCC. Drugs such as belzutifan have shown encouraging results in clinical settings by disrupting this pathway, particularly in patients with VHL-associated tumors. By curbing the expression of lipid uptake and synthesis proteins, these inhibitors aim to starve the tumor of essential resources needed for membrane formation and energy production. This approach represents a shift from traditional therapies, focusing on the metabolic underpinnings of cancer rather than just its proliferative capacity. The potential to slow disease progression through such targeted disruption is a significant step forward in managing this aggressive malignancy.
Another avenue involves directly reducing lipid accumulation through compounds that modulate key metabolic pathways, offering a promising strategy in the battle against certain cancers. Liver X receptor (LXR) agonists and inverse agonists, such as LXR623 and SR9243, work to lower cholesterol and fatty acid levels by altering the activity of regulatory proteins. Similarly, statins, which inhibit HMG-CoA reductase, are being explored for their ability to curb cholesterol synthesis and potentially impede tumor metastasis. These agents not only limit the tumor’s structural components but also sensitize it to other treatments by weakening its metabolic foundation. Challenges remain, including the risk of tumors adapting by tapping alternative fuel sources and the need to minimize impact on normal tissues. Nevertheless, the momentum behind lipid-focused therapies signals a growing recognition of metabolism as a viable target in the fight against clear cell renal cell carcinoma (ccRCC).
Harnessing Ferroptosis for Cancer Cell Destruction
Inducing ferroptosis in clear cell renal cell carcinoma represents a novel therapeutic strategy that capitalizes on the tumor’s lipid-heavy profile to trigger lethal oxidative damage, offering a promising avenue for treatment. Compounds like erastin target the system xc⁻ antiporter, blocking cystine uptake and depleting glutathione levels, which leaves lipid peroxides unchecked to destroy cell membranes. Given the abundance of polyunsaturated fatty acids in ccRCC cells, this approach can be particularly devastating, turning a metabolic trait into a fatal flaw. RSL3, another ferroptosis inducer, directly inhibits GPX4, stripping away a key defense against peroxidation. Preclinical studies demonstrate the potency of these agents in lipid-rich tumor models, suggesting a powerful tool to combat ccRCC’s resilience. The specificity of ferroptosis to cancer cells with high lipid content offers a unique angle for treatment development.
Yet, translating ferroptosis inducers into effective clinical therapies is fraught with obstacles that must be navigated carefully, as issues such as poor solubility and metabolic instability often hinder these compounds from reaching tumor sites in sufficient concentrations. Off-target effects also risk toxicity to healthy tissues. Normal cells, particularly immune components like CD8+ T cells, can be vulnerable to ferroptosis, potentially undermining the body’s anti-cancer defenses. Innovations like nanotechnology, with delivery systems such as MIL-101(Fe) nanoparticles, aim to address these limitations by ensuring precise targeting. Emerging agents like moscatilin are also under investigation for their ability to selectively induce ferroptosis in tumor cells. Despite the hurdles, the prospect of exploiting a metabolic weakness inherent to ccRCC keeps this field at the forefront of oncology research.
Combining Metabolic and Oxidative Stress Approaches
The integration of lipid metabolism inhibitors with ferroptosis inducers presents a synergistic strategy to combat clear cell renal cell carcinoma by attacking the tumor on multiple fronts. By pairing agents like HIF-2α inhibitors with compounds such as erastin, it’s possible to disrupt lipid stockpiling while simultaneously dismantling antioxidant defenses. This dual assault aims for synthetic lethality, where the combined stress becomes insurmountable for cancer cells. Preclinical evidence suggests that such combinations can significantly amplify cell death compared to standalone treatments, offering a pathway to tackle the tumor’s adaptability. This approach also holds potential to address resistance mechanisms that often undermine single-agent therapies, marking a strategic evolution in cancer management.
Further enhancing this synergy, combining metabolic targeting with existing treatments like tyrosine kinase inhibitors (TKIs) or immunotherapies can overcome barriers to efficacy, making it a promising strategy for improved outcomes in cancer treatment. Ferroptosis induction, for instance, can counteract the antioxidant upregulation that renders TKIs like sunitinib less effective over time. Additionally, ferroptosis-driven immunogenic cell death (ICD) releases signals that activate immune responses, pairing well with checkpoint inhibitors such as anti-PD-1 drugs to boost anti-tumor immunity. However, the complexity of these combinations demands precision to avoid toxicity, as multiple agents increase risks to normal tissues. Personalized medicine, supported by multi-omics data, could guide the tailoring of such regimens to individual tumor profiles, ensuring maximum impact. The promise of these combined approaches lies in their ability to target clear cell renal cell carcinoma (ccRCC) from diverse angles, reshaping treatment paradigms.
Navigating Barriers to Clinical Implementation
Bringing lipid reprogramming and ferroptosis-based therapies into clinical practice for clear cell renal cell carcinoma faces significant challenges that temper the excitement of preclinical successes. Tumors often exhibit remarkable plasticity, adapting to metabolic blockades by exploiting alternative energy sources, which can diminish the impact of lipid inhibitors. Ferroptosis inducers, meanwhile, grapple with practical limitations such as poor solubility and rapid degradation, reducing their ability to penetrate tumors effectively. Systemic toxicity remains a persistent concern, as both types of therapies can inadvertently affect healthy tissues reliant on similar lipid pathways. These hurdles underscore the gap between promising lab results and real-world application, necessitating innovative solutions to bridge this divide.
Another layer of complexity arises from the tumor microenvironment, which can modulate therapeutic responses in unpredictable ways, adding to the challenges of treatment development. Metabolites and immune-suppressive signals within this milieu may counteract the effects of lipid inhibition or ferroptosis induction, requiring strategies that account for these external influences. Patient variability also complicates matters, as not all ccRCC tumors display uniform metabolic profiles or ferroptosis resistance, demanding tailored approaches over generic solutions. Economic factors, including the high cost of developing novel agents and delivery systems like nanotechnology, pose additional barriers to accessibility. Despite these obstacles, ongoing advancements in drug design, targeted delivery, and patient stratification offer pathways forward, ensuring that the potential of metabolic therapies isn’t lost to practical constraints.
Immune Interactions Shaped by Lipid Metabolism
Lipid reprogramming in clear cell renal cell carcinoma extends its influence beyond tumor cells, profoundly shaping the surrounding immune landscape to favor cancer survival. Specific lipid metabolites, such as ganglioside GM2, can directly impair T-cell function by inducing apoptosis, thus weakening the body’s natural anti-cancer defenses. Similarly, apolipoprotein C1 (APOC1) drives macrophages toward an M2 phenotype, which promotes an immunosuppressive environment conducive to tumor growth. These immune-modulating effects are a direct byproduct of the tumor’s altered lipid metabolism, creating a barrier to effective immune surveillance. Targeting these lipid pathways could potentially reverse such immunosuppression, restoring the immune system’s ability to fight the cancer and offering a complementary angle to traditional therapies.
The intersection of lipid metabolism and immunity offers promising opportunities to improve immunotherapy outcomes in clear cell renal cell carcinoma (ccRCC), a common type of kidney cancer that often presents unique challenges in treatment. Ferroptosis induction, for instance, triggers immunogenic cell death, releasing molecular signals that activate dendritic cells and T cells, thereby amplifying immune responses. When paired with checkpoint inhibitors, this effect could significantly boost anti-tumor immunity. However, caution is necessary, as ferroptosis therapies risk harming beneficial immune cells, such as CD8+ T cells, which are also susceptible to lipid peroxidation. Balancing tumor targeting with immune preservation remains a critical challenge. As research deepens into immune-metabolic crosstalk, the possibility of reshaping the tumor microenvironment through lipid-focused interventions emerges as a compelling frontier for enhancing treatment efficacy.
Future Horizons in Metabolic Cancer Therapy
Looking back, the exploration of lipid reprogramming in clear cell renal cell carcinoma revealed a complex metabolic landscape that both fueled tumor growth and exposed critical vulnerabilities, painting a vivid picture of cancer’s adaptability. The journey through altered lipid uptake, synthesis, and resistance to ferroptosis portrayed cancer cells as metabolic opportunists, stockpiling fats to thrive. Therapeutic strategies, from HIF-2α inhibitors to ferroptosis inducers like erastin, demonstrated remarkable potential in preclinical models to disrupt this cycle. Combinations with immunotherapy and tyrosine kinase inhibitors further showcased how multi-pronged approaches tackled resistance, leveraging the tumor’s own traits against it. These efforts laid a foundation for a new understanding of ccRCC as a metabolically driven disease, where targeting lipid pathways offered a fresh perspective on treatment.
Moving forward, the focus must shift to actionable steps that refine these insights into tangible benefits for patients, ensuring that innovative approaches are both practical and impactful. Prioritizing clinical trials that test combination therapies with precision delivery systems, such as nanotechnology, can address past challenges like toxicity and poor tumor penetration. Integrating multi-omics profiling to customize treatments to individual metabolic signatures will ensure therapies hit their mark. Additionally, exploring the broader immune-metabolic interplay could unlock ways to bolster anti-tumor immunity without compromising essential defenses. The road ahead involves not just overcoming technical barriers but also ensuring accessibility through cost-effective solutions. By building on the groundwork established, the field stands poised to transform renal cancer therapy into a more targeted, effective discipline over the coming years.