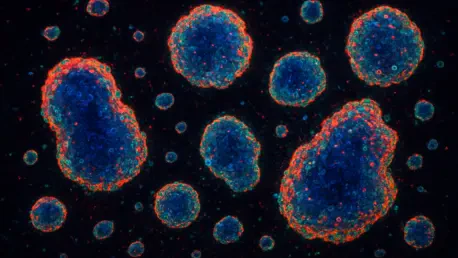
Colorectal cancer (CRC) stands as a formidable global health challenge, ranking as the third most common cancer and the second leading cause of cancer-related deaths worldwide, according to GLOBOCAN 2020 data with a 10.0% incidence rate and a 9.4% mortality rate. Within the complex landscape of this disease, a small subset of cells known as cancer stem cells (CSCs) plays a pivotal role by driving tumor initiation, persistence, and resistance to treatment through their ability to self-renew and differentiate. These cells are deeply influenced by the tumor microenvironment (TME), a dynamic network of stromal cells, blood vessels, and immune components that interact with cancer cells to fuel tumor growth and metastasis. Among the key players in the TME are mesenchymal stem cells (MSCs), particularly those derived from human umbilical cords (huc-MSCs), which exhibit both tumor-promoting and inhibiting effects through intricate signaling mechanisms. Recent research has shed light on how huc-MSCs interact with colorectal cancer stem cells (CCSCs) via indirect cell-cell contact, revealing potential pathways such as the PI3K/AKT signaling cascade that could unlock new therapeutic targets. This exploration delves into the mechanisms by which stem cells, particularly through these interactions, contribute to CRC progression, offering insights into the biological functions that sustain this deadly malignancy.
1. Unraveling the Role of Stem Cells in Colorectal Cancer
The significance of cancer stem cells in colorectal cancer cannot be overstated, as these cells are believed to be the root of tumor formation and recurrence due to their unique capacity for self-renewal and differentiation. Unlike typical cancer cells, CSCs can regenerate the entire tumor mass even after aggressive treatments, making them a primary reason why CRC remains difficult to eradicate. These cells reside within a specialized niche in the tumor microenvironment, where they receive critical signals from surrounding stromal and immune components that regulate their behavior. Research indicates that interactions within this environment not only sustain CSC survival but also enhance their ability to drive tumor expansion and resist conventional therapies. Understanding these dynamics is essential for developing strategies to disrupt the support systems that perpetuate CRC growth. The focus on CSCs has thus shifted attention to the broader ecosystem of the tumor, where non-malignant cells play unexpectedly influential roles.
Mesenchymal stem cells, especially those sourced from human umbilical cords, have emerged as significant modulators within the tumor microenvironment of colorectal cancer. These hUC-MSCs are known for their pluripotent nature and their ability to migrate toward tumor sites through chemotaxis, interacting with cancer cells via paracrine signaling. Studies have demonstrated that hUC-MSCs can promote colorectal cancer (CRC) progression by altering the biological functions of cancer cells, including proliferation and migration, while also exhibiting conflicting anti-tumor properties under certain conditions. This dual nature underscores the complexity of MSC involvement in cancer and highlights the need for precise investigations into their specific interactions with colorectal cancer stem cells (CCSCs). Such interactions, particularly through indirect cell-cell contact, appear to enhance tumor-supporting mechanisms, providing a fertile ground for exploring novel intervention points in CRC management.
2. Objectives Behind Investigating Stem Cell Interactions
The primary aim of recent studies has been to dissect the impact of human umbilical cord-derived mesenchymal stem cells on the growth and behavior of colorectal cancer cells. This involves a detailed examination of how huc-MSCs influence key processes such as proliferation, programmed cell death (apoptosis), cell cycle progression, and migration in CRC cells. By focusing on these fundamental biological functions, researchers seek to uncover the specific ways in which stem cell interactions exacerbate tumor development. The emphasis on indirect contact mechanisms provides a unique perspective on how paracrine signaling, rather than direct physical interaction, can significantly alter cancer cell dynamics. These insights are crucial for identifying potential vulnerabilities in CRC that could be targeted to halt its progression.
Beyond basic cellular functions, another critical objective is to explore how interactions between CRC cells and huc-MSCs affect angiogenesis, the process of new blood vessel formation that tumors rely on for growth and nutrient supply. This involves analyzing the balance of pro-angiogenic and anti-angiogenic factors released during co-culture experiments to understand how huc-MSCs might tip the scales in favor of tumor vascularization. Additionally, the influence of MSCs on the stemness of colorectal cancer stem cells is assessed through specialized assays like sphere formation, which measure the ability of CCSCs to maintain their self-renewal capacity. The role of huc-MSCs in promoting invasion and epithelial-mesenchymal transition (EMT)—a process linked to metastasis—is also a key focus, as is the activation of signaling pathways such as PI3K/AKT, which are implicated in driving tumor aggressiveness. Together, these objectives aim to build a comprehensive picture of stem cell-driven CRC growth.
3. Methodological Approaches to Study Stem Cell Effects
To investigate the intricate relationship between huc-MSCs and colorectal cancer, a robust methodology centered on cell culture techniques has been employed. The process begins with the collection of human umbilical cord samples from full-term pregnancies, conducted under strict ethical approval and with informed consent from donors. These samples are meticulously rinsed with phosphate-buffered saline (PBS) to eliminate blood contamination, then cut into 2-cm segments to facilitate the removal of the amnion, veins, and arteries. The gelatinous tissue is extracted and chopped into small fragments (0.5–1 mm³), which are placed into plastic flasks and incubated for 5 hours before the addition of Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% fetal bovine serum (FBS). The cells are maintained at 37°C in a humidified atmosphere with 5% CO₂, with the medium refreshed every 3 days, and passaged using trypsin when reaching approximately 80% confluence. This controlled environment ensures the viability and purity of huc-MSCs for subsequent experiments.
Further validation of huc-MSC properties involves differentiation testing for osteogenesis and adipogenesis. For osteogenesis, third-generation huc-MSCs are seeded in 6-well plates at a density of 2×10⁴ cells per well, and at 40% confluence, the medium is replaced with an osteogenic induction mix to initiate the process. On day 14, cells are fixed with paraformaldehyde, washed with PBS, and stained with Alizarin Red S to detect mineralized nodules indicative of bone formation. For adipogenesis, huc-MSCs are seeded at 2×10⁵ cells per well, and at 100% confluence, the medium is switched to an adipogenic induction mix, refreshed every 3 days. On day 14, cells are fixed, washed with PBS, and stained with Oil Red O to observe lipid droplet accumulation under a microscope. These tests confirm the multipotent nature of huc-MSCs, ensuring their suitability for studying interactions with CRC cells.
The co-culture setup is a critical component of the methodology, utilizing Transwell chambers with a 0.4 μm pore size to enable indirect contact between huc-MSCs and CRC cells, ensuring precise experimental conditions. In this system, huc-MSCs suspended in DMEM are placed in the upper chamber, while CRC cells are cultured in the lower chamber. After 24 hours of co-culture, the CRC cells are collected for detailed functional and mechanistic analyses. Additionally, conditioned medium preparation involves culturing 1×10⁶ MSCs, rinsing them with PBS, and incubating them in low-sugar DMEM with 10% FBS for 48 hours at 37°C. The medium is then centrifuged at 4°C for 5 minutes at 1000g, and the supernatant is stored at -20°C as MSC-conditioned medium (MSC-CM). This approach allows for the study of paracrine effects without direct cell contact.
Sphere formation assays are also employed to assess the stemness of CCSCs under the influence of huc-MSCs, providing critical insights into their behavior and potential therapeutic applications. CRC single-cell suspensions are seeded into ultra-low attachment 6-well plates at 5×10³ cells per well in FBS-free DMEM supplemented with growth factors. The cells are cultured for 7 days at 37°C with 5% CO₂, with the medium renewed every 3 days, and spheres ranging from 20 to 150 μm are counted under a microscope to evaluate self-renewal capacity. Complementary assays, including cell viability (MTT assay), flow cytometry for immunophenotyping and apoptosis, wound healing, migration, colony formation, EdU staining for proliferation, qPCR, Western blotting, tube formation for angiogenesis, and in vivo tumor studies in nude mice, provide a multifaceted analysis of stem cell interactions in CRC. This comprehensive methodology ensures a thorough understanding of the underlying mechanisms.
4. Key Discoveries on Stem Cell Influence in CRC
One of the most striking findings from recent research is the profound effect of huc-MSCs on colorectal cancer cell growth and survival through indirect co-culture systems. Experiments utilizing MTT assays, EdU staining, and colony formation tests have revealed a significant increase in CRC cell proliferation when exposed to huc-MSCs. Concurrently, flow cytometry data show a marked reduction in apoptosis, characterized by decreased levels of pro-apoptotic proteins like Bax and Caspase-3, alongside an increase in the anti-apoptotic protein Bcl-2. These results suggest that huc-MSCs create a protective environment for CRC cells, enabling them to thrive and resist programmed cell death. This enhanced survival capacity is a critical factor in the aggressive nature of CRC and underscores the tumor-supportive role of stem cells within the TME.
Another pivotal discovery concerns the alteration of the cell cycle in CRC cells under the influence of huc-MSCs. Flow cytometry analysis indicates a higher proportion of cells in the S-phase, which is associated with DNA synthesis and active division, following indirect co-culture. This shift is accompanied by a downregulation of key cell cycle inhibitors such as P53, P16, and P21, which normally restrain unchecked cell growth. By diminishing these regulatory barriers, huc-MSCs facilitate a more rapid progression through the cell cycle, thereby amplifying the proliferative potential of CRC cells. This mechanism highlights how stem cell interactions can directly contribute to tumor expansion by manipulating fundamental cellular processes.
The promotion of angiogenesis by huc-MSCs represents a critical finding, as tumors depend on new blood vessel formation for sustained growth, and understanding this mechanism could be key to developing targeted therapies. Co-culture experiments have demonstrated elevated levels of pro-angiogenic factors like IL-6 and VEGFA in CRC cells, coupled with a reduction in the anti-angiogenic factor IL-10. These molecular changes correlate with enhanced tube formation in human umbilical vein endothelial cells (HUVECs), indicating a heightened capacity for vascularization. Such alterations in the angiogenic profile suggest that huc-MSCs play a significant role in creating a tumor-friendly vascular network, ensuring a steady supply of nutrients and oxygen to support CRC progression. This aspect of stem cell influence is particularly concerning given its implications for tumor metastasis.
5. Enhancing Cancer Stem Cell Properties
Indirect contact with huc-MSCs has been shown to significantly enhance the stemness of colorectal cancer stem cells, a property central to their role in tumor initiation and persistence. Sphere formation assays reveal a notable increase in both the number and size of spheres formed by CCSCs after co-culture, reflecting a boosted self-renewal capacity. Additionally, Western blotting analysis indicates elevated expression of stemness markers such as CD133 and CD44 in these cells, further confirming the reinforcing effect of huc-MSCs on CSC characteristics. This enhancement of stem-like properties suggests that the tumor microenvironment, shaped by MSC interactions, actively sustains a population of highly malignant cells capable of driving CRC recurrence and resistance to therapy.
The impact of huc-MSCs on invasion and epithelial-mesenchymal transition (EMT) in CCSCs is equally significant, as these processes are closely linked to metastatic potential. Co-culture studies demonstrate increased migration in CRC cells and heightened invasion in CCSC-enriched populations, accompanied by molecular changes indicative of EMT. Specifically, there is a reduction in the epithelial marker E-cadherin and an upregulation of mesenchymal markers like N-cadherin and Vimentin. These shifts signify a transition to a more invasive phenotype, facilitated by the paracrine effects of huc-MSCs, which likely contribute to the spread of CRC to distant sites. Understanding these interactions offers critical insights into the mechanisms behind cancer dissemination.
6. Signaling Pathways and Tumor Growth In Vivo
A key mechanism through which huc-MSCs exert their tumor-promoting effects on CCSCs is the activation of the PI3K/AKT signaling pathway, which plays a critical role in cancer progression. Immunoblotting analyses reveal increased phosphorylation of PI3K and AKT in CCSCs following indirect co-culture with huc-MSCs, while total levels of these proteins remain unchanged. This heightened activation drives multiple aspects of tumor progression, including cell survival, proliferation, and resistance to apoptosis. The PI3K/AKT pathway’s role as a central regulator of these processes underscores its potential as a therapeutic target, as inhibiting this signaling could disrupt the supportive effects of huc-MSCs on CRC. This finding provides a molecular basis for the observed enhancements in tumor aggressiveness.
In vivo studies further confirm the tumor-promoting role of huc-MSCs, with CCSCs co-cultured with huc-MSCs forming larger and more invasive tumors in nude mice compared to controls. These tumors exhibit faster initiation times, often becoming palpable within 7 days post-injection, and display abundant surface vasculature and a harder texture. Molecular analyses of the tumor tissues reveal elevated expression of stemness markers (CD133, CD44, OCT4, SOX2) and EMT-related markers, alongside increased phosphorylation of PI3K/AKT pathway components. These results indicate that indirect interactions with huc-MSCs significantly enhance the malignant phenotype of CCSCs, validating in vitro findings and highlighting the real-world implications of stem cell-driven CRC growth.
7. Insights and Limitations of Current Research
Comparative analysis with prior research reveals that the tumor-promoting effects of huc-MSCs align with findings on other MSC types, such as bone marrow-derived MSCs, which also influence cancer through paracrine signaling. These studies collectively suggest that MSCs modulate critical processes like cell cycle progression and apoptosis inhibition through secreted factors that alter the tumor microenvironment. The current data on huc-MSCs extend this understanding by demonstrating specific impacts on CRC cell proliferation, migration, and angiogenesis, mediated by shifts in molecular regulators. Such consistency across different MSC sources reinforces the notion that stem cells are integral to cancer dynamics, shaping therapeutic resistance and disease progression in predictable yet complex ways.
Despite these advances, limitations in the scope of current research must be acknowledged, particularly the exclusive focus on indirect co-culture models. While this approach effectively highlights paracrine effects, it overlooks the potential contributions of direct cell-cell contact, which may elicit distinct responses in CRC and CCSCs. Future investigations should incorporate direct interaction studies to provide a more holistic view of MSC roles within the tumor microenvironment. Additionally, the dual nature of MSCs—exhibiting both pro- and anti-tumor effects—requires further exploration to clarify context-dependent behaviors. Addressing these gaps will enhance the applicability of research findings to clinical settings, ensuring a comprehensive understanding of stem cell influences in CRC.
8. Looking Ahead: Implications for CRC Management
Reflecting on the extensive body of research, it is evident that human umbilical cord-derived mesenchymal stem cells play a substantial role in enhancing colorectal cancer cell growth, migration, and angiogenesis through indirect cell-cell contact. These interactions, which bolster the stemness of colorectal cancer stem cells and activate critical pathways like PI3K/AKT, are instrumental in driving tumor progression both in vitro and in vivo. The molecular shifts observed, including those related to epithelial-mesenchymal transition, underscore how huc-MSCs reshape the tumor microenvironment to favor malignancy. These findings, documented through rigorous experimental approaches, lay a foundation for rethinking traditional CRC treatment paradigms by highlighting the overlooked influence of non-malignant cells in cancer dynamics.
Moving forward, the insights gained from these studies suggest actionable strategies for managing colorectal cancer, starting with the potential targeting of CCSC-huc-MSC interactions to disrupt tumor-supportive networks. Developing therapies aimed at inhibiting the PI3K/AKT signaling pathway could offer a promising avenue to counteract the aggressive traits imparted by huc-MSCs. Moreover, expanding research to include direct contact effects and exploring the dual roles of MSCs in various contexts will be crucial for translating these findings into clinical applications. By fostering a deeper understanding of stem cell contributions to the tumor microenvironment, future efforts can pave the way for innovative treatments that address the root causes of CRC persistence and spread, ultimately improving patient outcomes.