Picture a medical landscape where treatments can slip past the body’s toughest defenses, delivering healing payloads directly to diseased cells without harming the surrounding healthy tissue. This isn’t science fiction but the tantalizing promise of engineered exosomes—tiny biological couriers that could redefine how therapies reach their targets. These naturally occurring vesicles, once dismissed as mere cellular debris, have emerged as powerful tools in biopharmaceutical innovation. Their potential to carry complex drugs across barriers like the blood-brain barrier positions them as game-changers in treating conditions previously deemed untreatable. This FAQ article aims to unpack the transformative role of engineered exosomes in targeted therapies, addressing key questions about their capabilities, challenges, and future impact. Readers can expect to explore how these microscopic marvels work, the hurdles they face, and the profound implications for precision medicine.
Key Questions About Engineered Exosomes
What Are Engineered Exosomes and Why Do They Matter?
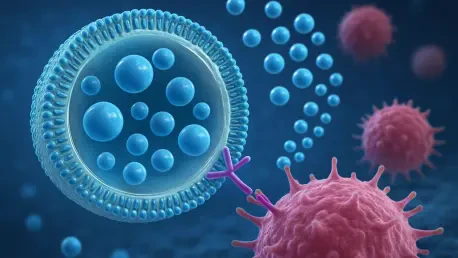
At their core, exosomes are small extracellular vesicles secreted by nearly all cell types, acting as natural messengers that shuttle proteins, RNA, and other molecules between cells. Their engineered counterparts are modified through scientific techniques to enhance their ability to carry therapeutic cargos and target specific tissues. This matters immensely because traditional drug delivery methods often struggle with biological barriers and cause unintended side effects due to non-specific distribution. Engineered exosomes, with their inherent biocompatibility and low risk of triggering immune responses, offer a safer, more precise alternative. Their significance lies in unlocking treatments for hard-to-reach areas like the brain or dense tumor environments, potentially revolutionizing care for neurological disorders and cancer.
Delving deeper, the ability of exosomes to cross barriers that stymie other delivery systems—such as the blood-brain barrier—makes them a beacon of hope for conditions like Alzheimer’s or glioblastoma. Unlike synthetic nanoparticles, which can provoke inflammation, exosomes are naturally equipped to blend into the body’s landscape. By tweaking their surfaces or the cells that produce them, scientists can load them with diverse therapies, from gene-editing tools to RNA molecules, paving the way for bespoke medical solutions. This adaptability underscores why they’re seen as a cornerstone of next-generation drug delivery, promising to expand the realm of what’s treatable.
How Do Engineered Exosomes Improve Drug Delivery Precision?
Precision in drug delivery has long been a holy grail in medicine, and engineered exosomes are stepping up to the challenge. Naturally, exosomes interact with cells through specific surface markers, but in their unmodified form, they lack the focus needed for therapeutic use. Engineering techniques, such as attaching targeting ligands or modifying source cells genetically, allow these vesicles to home in on particular tissues or cell types with remarkable accuracy. This means a cancer drug could be directed straight to tumor cells, minimizing collateral damage to healthy tissue, or a neurological therapy could reach brain cells without scattering throughout the body.
Moreover, this precision addresses a critical flaw in conventional therapies: off-target effects that often lead to toxicity. By enhancing stability and preventing rapid clearance from the bloodstream, engineered exosomes ensure that more of the therapeutic payload reaches its intended destination. For example, studies have shown that exosomes modified with specific peptides can penetrate dense tumor microenvironments, delivering anti-cancer agents more effectively than traditional methods. This capability not only boosts efficacy but also reduces the dosage required, potentially cutting down on side effects and improving patient outcomes. The ripple effect of such advancements could redefine treatment protocols across multiple disease areas.
What Types of Therapies Can Engineered Exosomes Deliver?
The versatility of engineered exosomes is one of their most exciting attributes. They can be loaded with a wide array of therapeutic cargos, ranging from nucleic acids like messenger RNA and small interfering RNA to proteins and even sophisticated gene-editing systems such as CRISPR/Cas. This broad applicability positions them as a platform technology capable of addressing diverse medical challenges. Whether it’s silencing faulty genes in genetic disorders, replacing missing proteins in metabolic conditions, or editing DNA to combat cancer, exosomes offer a delivery vehicle that can adapt to the payload’s unique demands.
In addition, their natural ability to transfer complex molecules between cells makes them particularly suited for cutting-edge therapies where traditional systems falter. Consider neurodegenerative diseases: delivering treatments across the blood-brain barrier has historically been a stumbling block, but exosomes have shown promise in carrying therapeutic RNA to brain cells, opening new avenues for conditions like Parkinson’s. Their role isn’t limited to niche applications either; oncology, rare genetic diseases, and even cardiovascular conditions could benefit from tailored exosome-based interventions. As research progresses, the scope of therapies they can deliver continues to widen, hinting at a future where personalized medicine becomes the norm.
What Challenges Hinder the Clinical Use of Engineered Exosomes?
Despite their promise, engineered exosomes face significant roadblocks on the path to clinical application. One of the primary challenges is the heterogeneity of exosome populations, which complicates efforts to define their identity, purity, and potency. Current analytical tools often fall short in distinguishing exosomes from other vesicles or contaminants, making it tough to ensure consistent quality. This variability poses a dilemma for developers who need reliable metrics to predict how these therapies will behave in the human body, a crucial factor for gaining regulatory approval.
Furthermore, manufacturing at scale presents another hurdle. Producing engineered exosomes in quantities sufficient for widespread use involves navigating variables like cell source, culture conditions, and purification methods. Techniques that work in a lab setting, such as tangential flow filtration, often require extensive optimization to balance yield and cost when scaled up. Without standardized processes under good manufacturing practices, batch-to-batch inconsistency remains a persistent concern, stalling progress toward commercialization.
Lastly, regulatory frameworks have yet to catch up with this novel technology. The absence of harmonized standards across regions creates uncertainty for developers who must tailor their approaches to different agencies. Safety concerns, such as biodistribution and potential off-target effects, demand robust data that isn’t always easy to generate given current limitations in characterization. Overcoming these analytical, bioprocessing, and regulatory barriers will be essential to translating the theoretical advantages of exosomes into real-world therapies.
What Impact Could Successful Exosome Therapies Have on Medicine?
If the challenges are surmounted, the impact of engineered exosome therapies on medicine could be nothing short of revolutionary. By enabling precise delivery of complex treatments, they have the potential to expand the range of conditions that can be effectively addressed, particularly those constrained by delivery issues. Diseases of the central nervous system, dense cancers, and rare genetic disorders could see new therapeutic options, shifting clinical approaches toward highly targeted interventions that minimize harm to healthy tissues.
Beyond patient outcomes, their success would likely reshape the biopharmaceutical industry itself. The demand for specialized manufacturing systems, standardized cell lines, and advanced purification workflows could spur innovation in supply chains, though it would also require substantial investment. Clinical trial designs might need retooling to account for delivery-dependent outcomes, and companion diagnostics could become integral to identifying suitable patients. Economically and scientifically, the ripple effects would be profound, positioning exosomes as a catalyst for a new era of precision medicine.
Additionally, regulatory landscapes would evolve in response to these therapies. Agencies would need to develop clear guidelines for evaluating heterogeneous vesicle preparations, ensuring safety and efficacy are adequately demonstrated. This adaptation could set precedents for other advanced therapies, streamlining future innovations. The broader implication is a healthcare system where treatments are not just reactive but finely tuned to individual biological needs, heralding a transformative shift in how diseases are managed.
Summary of Key Insights
Engineered exosomes stand as a beacon of innovation in targeted therapies, blending natural biological properties with scientific enhancements to deliver treatments with unprecedented precision. This FAQ has explored their definition and importance, highlighting their role as customizable vehicles for a range of therapies, from RNA to gene-editing tools. Their ability to improve drug delivery accuracy, traverse tough biological barriers, and adapt to diverse medical needs underscores their potential to redefine treatment landscapes. Challenges like analytical inconsistencies, manufacturing scalability, and regulatory ambiguity remain significant, yet the prospective impact on medicine—spanning clinical, economic, and systemic shifts—paints a compelling picture of what’s at stake.
The main takeaway is that while engineered exosomes are not yet a clinical reality for widespread use, their promise in expanding the druggable space and enhancing patient outcomes is undeniable. For those eager to dive deeper, exploring resources from biopharmaceutical journals or industry reports on extracellular vesicles can provide further insight into ongoing research and development efforts. Staying informed about advancements in this field offers a glimpse into the future of personalized healthcare.
Final Thoughts
Reflecting on the discussions held, it became clear that engineered exosomes held immense potential to alter the trajectory of medical treatments, offering solutions where traditional methods stumbled. The journey to overcome their technical and systemic obstacles proved to be a complex endeavor, yet the vision of targeted, efficient therapies drove relentless innovation. Their ability to navigate the body’s defenses and deliver precise interventions sparked hope for countless patients who faced limited options.
Looking ahead, the focus must shift to collaborative efforts between researchers, industry leaders, and regulators to iron out the kinks in production and oversight. Investing in advanced analytical tools and scalable manufacturing processes should take priority to ensure consistency and safety. For individuals and stakeholders in healthcare, considering how these developments might address specific unmet needs or influence future treatment strategies is a valuable next step. The road may be long, but the destination—a world of truly personalized medicine—offers a compelling reason to push forward.