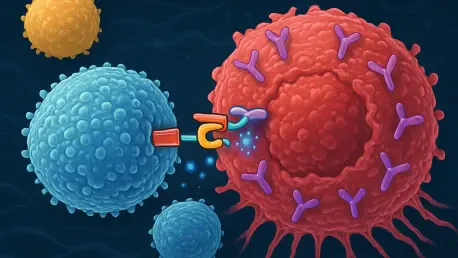
In the rapidly evolving landscape of cancer treatment, few innovations have captured as much attention as chimeric antigen receptor T cell (CAR-T) therapy, a groundbreaking method that reprograms a patient’s immune cells to attack cancer with remarkable precision. Originally developed as a niche treatment for specific blood cancers, CAR-T has demonstrated curative potential, igniting hope for its broader application across various diseases. Yet, despite its transformative promise, a staggering 80% of eligible patients currently miss out on this life-changing therapy due to a web of logistical, financial, and systemic barriers. Many are forced to travel vast distances to specialized centers, while others grapple with insurance limitations, particularly those relying on Medicaid or Medicare. At a recent industry gathering in Phoenix, Arizona, experts convened to address the critical challenge of transitioning CAR-T from a limited, specialized option to a foundational element of cancer care. The urgency to overhaul access and delivery models has never been clearer, as the potential to save countless lives hangs in the balance.
Overcoming the Access Gap
A fundamental hurdle in mainstreaming CAR-T therapy lies in dismantling the barriers that prevent most eligible patients from receiving it. The current model, heavily reliant on a limited number of academic medical centers, creates significant logistical challenges, often requiring patients to travel hundreds of miles for treatment. This burden disproportionately affects those in rural or underserved areas, where access to specialized care is scarce. Industry leaders advocate for decentralizing delivery, envisioning a future where community hospitals and outpatient clinics can administer CAR-T therapy. Such a shift could dramatically expand reach, ensuring that geography no longer dictates a patient’s chance at treatment. However, this transition demands careful planning to equip smaller facilities with the necessary resources and expertise, as the complexity of CAR-T administration cannot be understated. Without robust support systems, decentralization risks becoming an unfulfilled promise rather than a practical solution.
Financial constraints further compound the access issue, with many patients facing insurmountable costs despite the therapy’s potential to offer long-term value as a one-time treatment. For the significant portion of the population dependent on government-funded insurance programs like Medicaid or Medicare, volatile policy environments and reimbursement uncertainties often stand in the way. Addressing these challenges requires not just innovative care models but also policy reforms to stabilize funding and ensure equitable access. Collaboration with payers to streamline approval processes could alleviate some of the burden, while advocacy for broader coverage might help bridge the gap for underserved groups. The vision of bringing CAR-T closer to patients’ homes is compelling, but it must be underpinned by systemic changes that tackle both logistical and economic obstacles. Only through such comprehensive efforts can the therapy begin to reach the vast majority of those who stand to benefit from its remarkable outcomes.
Safeguarding Quality in New Care Models
As CAR-T therapy edges toward broader implementation in community and outpatient settings, ensuring consistent quality and safety emerges as a critical priority. Unlike traditional treatments, CAR-T involves highly specialized processes and carries risks of severe side effects, such as cytokine release syndrome and neurotoxicity, which demand expert management. Organizations like the Foundation for the Accreditation of Cellular Therapy (FACT) are stepping up to revise standards, crafting guidelines that are “fit-for-purpose” for diverse care environments. These updated frameworks aim to maintain rigorous safety protocols while adapting to the realities of smaller facilities that may lack the infrastructure of academic centers. The goal is to create a balance where accessibility does not come at the expense of patient well-being, ensuring that every treatment site meets a baseline of excellence.
Implementing these standards, however, is no small feat, as it requires training staff across varied settings and establishing partnerships between community providers and specialized hospitals for support during complex cases. The risk of adverse events necessitates continuous monitoring and rapid response capabilities, which can strain resources in less-equipped facilities. To address this, industry stakeholders are exploring innovative solutions, such as telemedicine integration for real-time consultation with experts and shared protocols to standardize care delivery. The emphasis on quality also extends to patient follow-up, as long-term monitoring is essential to assess the therapy’s durability and detect late-onset complications. By embedding robust safety mechanisms into new care models, the field can build trust among patients and providers alike, paving the way for CAR-T to become a reliable option beyond elite medical institutions. This focus on consistency is a cornerstone of transforming a niche treatment into a widely accepted standard.
Scaling Up Through Manufacturing Innovation
One of the most pressing challenges in expanding CAR-T therapy lies in manufacturing, where current methods struggle to keep pace with potential demand. Autologous therapies, which rely on harvesting and modifying a patient’s own cells, are labor-intensive and expensive, often placing the treatment out of financial reach for many. Industry leaders are increasingly turning their attention to allogeneic, or “off-the-shelf,” approaches that use donor cells to create ready-to-use doses, potentially slashing costs to a target range of $10,000 to $20,000 per treatment. This shift could be transformative, especially as CAR-T applications extend beyond blood cancers into areas like autoimmune diseases, which involve much larger patient populations. The ability to produce therapies at scale would not only improve access but also position CAR-T as a viable option for a wider array of conditions.
Yet, transitioning to allogeneic methods is not without hurdles, as these therapies must overcome issues of immune rejection and ensure comparable efficacy to their autologous counterparts. Research and development efforts are intensifying to refine these technologies, with companies investing heavily in advanced manufacturing platforms to boost efficiency. The durability of autologous treatments, often described as a “one-and-done” solution, remains a benchmark that allogeneic options must match to justify widespread adoption. Additionally, regulatory pathways for these newer approaches need to evolve to accommodate rapid scaling while maintaining stringent safety checks. The push for manufacturing innovation represents a pivotal step toward affordability and availability, addressing a core barrier to mainstreaming CAR-T. If successful, these advancements could redefine how cellular therapies are produced and delivered, unlocking their full potential for global impact.
Centering Patients in the Journey
Mainstreaming CAR-T therapy also hinges on placing patients at the core of the treatment process, ensuring their voices shape how care is designed and delivered. Many individuals facing cancer encounter not only physical challenges but also emotional and logistical burdens when navigating complex therapies like CAR-T. Listening to their experiences—whether it’s the stress of traveling for treatment or the uncertainty of insurance coverage—can guide the development of more compassionate and accessible systems. Patient advocacy groups emphasize the importance of addressing these real-world concerns, pushing for solutions that prioritize ease of access over administrative hurdles. By focusing on the human element, the healthcare ecosystem can build trust and encourage more patients to pursue this potentially life-saving option without fear of insurmountable obstacles.
Equally vital is the role of education in normalizing CAR-T as a standard treatment rather than an experimental novelty. Many referring physicians and patients remain unfamiliar with the therapy’s benefits and processes, leading to low referral rates and missed opportunities. Comprehensive training programs for healthcare providers can bridge this knowledge gap, equipping them to confidently discuss CAR-T as a viable choice. Simultaneously, clear, accessible information for patients can demystify the treatment, empowering them to make informed decisions with their doctors. This dual focus on education and patient-centered care aims to shift perceptions, transforming CAR-T from a distant, unattainable innovation into a routine part of cancer management. Such efforts are essential to driving uptake and ensuring that the therapy’s benefits reach those who need them most, regardless of background or circumstance.
Building a Collaborative Future
The journey to mainstream CAR-T therapy ultimately depends on robust collaboration across the entire healthcare ecosystem, uniting providers, payers, manufacturers, and advocates in a shared mission. Systemic barriers, from fluctuating insurance policies to regulatory complexities, cannot be addressed by any single entity alone. Joint efforts are needed to stabilize reimbursement models, ensuring that financial constraints do not exclude eligible patients from accessing treatment. Manufacturers must work with policymakers to streamline approval processes for new manufacturing techniques, while healthcare providers collaborate to refine delivery models that suit diverse settings. This interconnected approach is crucial for turning innovative ideas into tangible outcomes that reshape cancer care on a global scale.
Beyond logistics and policy, collaboration also means fostering a shared narrative that positions CAR-T as a cornerstone of modern medicine. Industry leaders stress the need for bold, transformative changes rather than incremental fixes, calling for a unified push to tackle deep-rooted challenges. Patient advocates play a key role in this dialogue, ensuring that clinical advancements align with real needs and experiences. By aligning goals and resources, stakeholders can address the multifaceted hurdles—financial, operational, and perceptual—that currently limit CAR-T’s reach. The consensus is clear: only through sustained, collective action can the therapy transition from a niche solution to a widely accessible standard. Looking back, the commitment shown by diverse voices at industry discussions reflected a pivotal moment, setting the stage for actionable strategies to ensure CAR-T’s promise becomes a reality for countless patients.