Managing severe, persistent respiratory conditions often feels like a relentless battle, with frequent treatments and the constant threat of debilitating flare-ups dictating the rhythm of daily life. For millions, conditions like severe asthma and chronic rhinosinusitis with nasal polyps represent not just a health issue but a significant barrier to a normal, active lifestyle. The recent European approval of a new biologic therapy, however, introduces a paradigm shift in treatment frequency, offering the potential for sustained control with an unprecedented twice-yearly dosing schedule. This change could profoundly impact how patients and clinicians approach long-term management of these complex inflammatory diseases.
This article serves as a comprehensive guide to understanding this new treatment, Exdensur (depemokimab). Its objective is to answer key questions surrounding its approval, mechanism of action, and the clinical evidence supporting its use. Readers can expect to gain a clear understanding of what this therapy is, who it is for, and why its ultra-long-acting nature marks a significant milestone in respiratory medicine. The following sections will break down its application in both severe asthma and chronic sinus conditions, providing the context needed to appreciate its potential impact.
Key Questions and Topics
What Is Exdensur and Why Is It a Breakthrough
Exdensur, the brand name for depemokimab, is a biologic therapy developed by GSK that has received authorization from the European Commission. It is designed to treat specific types of severe respiratory diseases that are driven by an underlying inflammatory process known as type 2 inflammation. The approval is a landmark event because Exdensur is the first and only ultra-long-acting biologic approved for respiratory conditions in the European Union. Its most distinguishing feature is its administration schedule, requiring only two injections per year to maintain its therapeutic effect.
This extended duration of action directly addresses a major challenge in managing chronic conditions: treatment burden. Patients with severe asthma or chronic rhinosinusitis with nasal polyps (CRSwNP) often require frequent medications, including other biologics that may be administered every few weeks or months. By providing six months of continuous disease control with a single dose, Exdensur simplifies the treatment regimen significantly. This not only enhances convenience but also has the potential to improve patient adherence and, consequently, long-term outcomes for those struggling with otherwise difficult-to-control symptoms.
Who Is Eligible for This New Treatment
The European Commission’s approval specifies two distinct patient populations who can benefit from Exdensur. The first group includes individuals aged 12 and older with severe asthma characterized by type 2 inflammation. This therapy is intended as an add-on maintenance treatment for patients whose asthma is not adequately managed with high-dose inhaled corticosteroids combined with another controller medication. For these individuals, frequent and severe asthma attacks, or exacerbations, remain a persistent threat despite their current treatment plan.
The second indication is for adults with severe chronic rhinosinusitis with nasal polyps. CRSwNP is a condition where growths in the nasal passages cause significant breathing difficulties, loss of smell, and poor sleep quality. Exdensur is approved as an add-on therapy for those whose condition remains uncontrolled even after treatment with systemic corticosteroids and/or nasal surgery. In both cases, the therapy targets patients with a high unmet need, offering a new option where previous treatments have failed to provide sufficient relief from their symptoms and the underlying inflammation.
How Does Exdensur Work so Infrequently
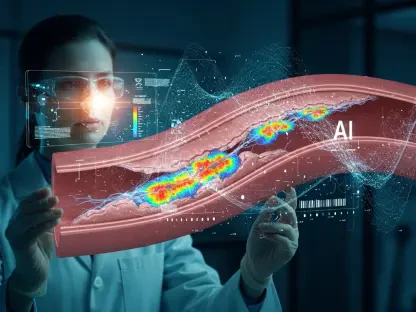
The ability of Exdensur to work effectively over a six-month period stems from its sophisticated biological design. The medication functions by targeting interleukin-5 (IL-5), a cytokine that plays a central role in promoting type 2 inflammation. This type of inflammation is characterized by the overproduction of eosinophils, a type of white blood cell that can cause tissue damage in the airways and nasal passages. By binding to IL-5 with high affinity, depemokimab prevents it from activating eosinophils, thereby suppressing the inflammatory cascade.
What makes it an ultra-long-acting therapy is its extended half-life, which means the drug remains active in the body for a much longer duration than other biologics. This prolonged activity allows a single dose to maintain control over eosinophilic inflammation for half a year. This mechanism was validated in a series of four large-scale Phase III clinical trials—SWIFT-1 and SWIFT-2 for severe asthma, and ANCHOR-1 and ANCHOR-2 for CRSwNP—all of which successfully demonstrated the drug’s ability to deliver statistically significant and clinically meaningful results over the extended dosing interval.
What Does the Clinical Evidence Show for Asthma
The effectiveness of Exdensur in treating severe asthma was convincingly demonstrated in the SWIFT-1 and SWIFT-2 trials. These studies focused on patients with a history of frequent exacerbations and elevated blood eosinophils. Over a 52-week period, patients receiving Exdensur experienced a dramatic reduction in the rate of asthma attacks compared to those on placebo. In the SWIFT-1 trial, the reduction was 58%, while the SWIFT-2 trial showed a 48% reduction, underscoring its consistent ability to protect patients from flare-ups.
Furthermore, a combined analysis of both trials revealed an even more profound impact on the most dangerous events. Exdensur reduced clinically significant exacerbations—those requiring hospitalization or an emergency room visit—by an impressive 72% compared to placebo. This finding is particularly important, as preventing severe attacks is a primary goal of asthma management. Crucially, across both pivotal studies, the safety profile of Exdensur was comparable to that of the placebo, indicating that its powerful efficacy did not come at the cost of increased risk, establishing a favorable risk-benefit balance.
How Effective Is It for Nasal Polyps
For adults with severe CRSwNP, the ANCHOR-1 and ANCHOR-2 trials provided robust evidence of Exdensur’s efficacy. The studies enrolled patients whose symptoms remained burdensome despite previous treatments, including surgery. The primary goals were to reduce the physical size of the nasal polyps and alleviate the debilitating symptoms they cause. Over the 52-week treatment period, patients receiving Exdensur showed a statistically significant reduction in their total nasal polyp score compared to the placebo group.
In addition to shrinking the polyps, the treatment also provided significant relief from one of the most disruptive symptoms: nasal obstruction. By the end of the study, patients reported notable improvements in their ability to breathe through their nose. This dual action—addressing both the underlying pathology and its symptomatic manifestation—highlights the therapy’s comprehensive benefit. For a condition that profoundly impacts quality of life by impairing breathing, smell, and sleep, an effective long-acting option represents a major therapeutic advancement.
Summary or Recap
The European approval of Exdensur (depemokimab) establishes a new benchmark in the management of severe type 2 inflammatory respiratory diseases. As the first ultra-long-acting biologic for these conditions, its twice-yearly dosing schedule offers a significant reduction in treatment burden for patients with severe asthma and chronic rhinosinusitis with nasal polyps. This innovative approach is designed to enhance convenience and adherence, ultimately supporting better long-term disease control.
Exdensur’s mechanism of action, which involves sustained suppression of interleukin-5, is backed by compelling clinical data from four Phase III trials. These studies confirm its ability to drastically reduce severe asthma exacerbations and improve the signs and symptoms of CRSwNP. With its favorable safety profile and proven efficacy, Exdensur stands as a transformative option for patients who have struggled to achieve control with existing therapies. This therapy’s availability in Europe, alongside recent approvals in other major global markets, reinforces a strategic shift toward long-acting treatments that simplify care for chronic conditions.
Conclusion or Final Thoughts
The authorization of Exdensur by the European Commission was more than a regulatory milestone; it represented a tangible shift in the philosophy of chronic disease management. It acknowledged that for patients whose lives are often defined by their treatment schedules, true innovation lies not only in efficacy but also in how seamlessly a therapy can integrate into their lives. The development of a biologic that provides six months of protection moved the goalposts from frequent intervention toward sustained, background control, allowing patients to focus less on their condition and more on their well-being.
This approval also underscored a broader trend in biopharmaceutical research toward creating therapies with extended durations of action, a pursuit that promised to reshape patient experiences across numerous therapeutic areas. Looking ahead, the exploration of depemokimab for other eosinophil-driven diseases, such as EGPA, HES, and certain types of COPD, suggested that the impact of this ultra-long-acting platform was only beginning. The journey from frequent to infrequent dosing marked a significant step forward in aligning medical science with the fundamental human desire for a less encumbered life.