Chronic HIV infection, even under suppressive antiretroviral therapy, can trap the immune system in a state of simmering alarm that never fully resolves and quietly erodes the fitness of the very T cells needed for durable control of the virus. That conundrum has intensified attention on the small but mighty plasmacytoid dendritic cells (pDCs), whose persistent type I interferon output can keep inflammation humming while blunting antiviral responses. A study from the Institute of Human Virology at the University of Maryland School of Medicine, published in Science Translational Medicine (Li et al., 2025), reports that tamping down overactive pDCs not only restores function in a key subset of CD8+ T cells but also contracts the HIV reservoir in experimental models. Moreover, combining this approach with a checkpoint inhibitor magnified immune recovery, pointing to a strategy that rebalances rather than simply revs the immune engine.
Rethinking Immune Activation in Chronic HIV
The Interferon Paradox And pDCs’ Double-Edged Role
For decades, type I interferons have been celebrated as frontline antiviral mediators that rally early defenses and choke viral replication before it spirals. In chronic HIV, however, the same signaling axis can become a liability: high-baseline interferon activity fosters tissue inflammation, sustains inhibitory pathways, and accelerates the drift of virus-specific T cells toward exhaustion. pDCs sit at the center of this paradox. Although rare in circulation, they disproportionately shape the interferon milieu, and when stuck in overdrive, they etch a proinflammatory set point that stabilizes the reservoir and undermines help from other immune partners. The new work reframes pDCs as strategic levers; tuning them down, rather than silencing them outright, recalibrates a system that has drifted from acute-phase defense to chronic self-sabotage.
By focusing on pDCs as a keystone node, the study helps reconcile puzzling observations that have lingered across cohorts on long-term therapy: why immune activation persists despite viral suppression and why T cells struggle to regain breadth, depth, and durability. The researchers show that curbing pDC-driven interferon signaling relaxes the inflammatory chokehold that narrows T cell options, especially for “stem-like” CD8+ T cells that seed long-lived responses. This subset is crucial because it can self-renew, differentiate into potent effectors on demand, and maintain control over time. When pDC output is tempered, these cells reemerge with improved functionality, suggesting that the problem is not a missing accelerator but an overbearing brake applied at the wrong time in the disease course.
Why Rebalancing Beats Brute-Force Stimulation
Traditional attempts to rescue antiviral immunity in chronic infection have leaned on generalized stimulation—more cytokines, more activation, more proliferation. Yet blunt force can backfire in a system already leaning into hyperactivation, further feeding exhaustion pathways and inadvertently fortifying the reservoir. The rebalancing concept explored here takes a different tack: dial down the pathologic signal that crowds out quality control, then allow adaptive immunity to recalibrate toward precision and persistence. Dampening pDC overactivity reduces interferon noise, lowers inflammatory collateral damage, and creates space for T cells to recover functional diversity without escalating burnout.
This precision approach mirrors lessons drawn from immuno-oncology, where timing, context, and cellular state determine whether an intervention energizes or exhausts. In the HIV setting, restraining pDCs appears to protect the stem-like compartment from continuous stress signals that would otherwise push it into dysfunction. As a result, CD8+ T cells regain the capacity to mount sustained responses, not merely transient bursts. The distinction matters for clinical translation: a therapy that privileges durability over amplitude could better complement antiretroviral backbones, curtail non-AIDS complications linked to inflammation, and open a path to reduce reservoir size without triggering damaging immune flares.
How the Study Tested the Idea
Models, Interventions, And Outcome Measures
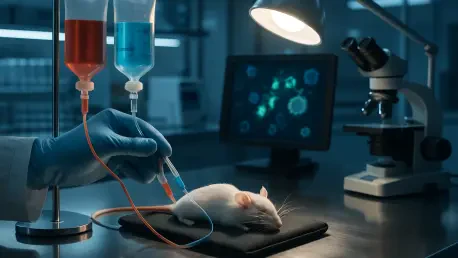
The research team built its case through a blend of preclinical rigor and human relevance. Humanized mouse models served as the mechanistic workbench, capturing core features of HIV pathogenesis, including reservoir formation and immune dysregulation under therapy. Within this system, the investigators selectively reduced overactive pDCs to see whether lowering interferon pressure would let antiviral T cells rebound. In parallel arms, they added an immune checkpoint inhibitor to lift exhaustion constraints and test whether the two maneuvers would work in concert or at cross-purposes. Readouts spanned systemic inflammation, interferon footprints, and, crucially, the function and phenotype of HIV-reactive stem-like CD8+ T cells, alongside quantitative measures of the reservoir.
The methods extended beyond mice. To anchor findings in human biology, the team analyzed blood from people with HIV on suppressive therapy, probing pDC activity, interferon signatures, and T cell states. Although these human data were correlative, they offered a translational mirror: similar immune patterns emerged where pDC signaling was pronounced, hinting that what played out in mice might also shape the immunologic landscape in treated infection. The alignment between models and human samples strengthened confidence that the intervention targets a genuine driver of dysfunction rather than a laboratory artifact, setting the stage for carefully designed clinical testing that respects the delicate role pDCs play in antiviral defense.
Evidence Across Systems Supports Clinical Relevance
Results converged on a coherent story. In humanized mice, moderating pDC activity muted chronic interferon cues, reduced inflammatory biomarkers, and revived the pool of stem-like CD8+ T cells with renewed capacity to proliferate and clear infected targets. These immunologic gains coincided with a measurable contraction of the HIV reservoir, indicating that the qualitative improvement in T cell function translated into pressure on persistence mechanisms. Importantly, the approach did not rely on sweeping immune activation; instead, it cleared static from a channel that had been broadcasting at the wrong volume for too long, allowing signal to carry without distortion.
Human blood analyses echoed the mechanistic insights by linking heightened pDC–interferon signatures with markers of T cell exhaustion and lower functional resilience. While not interventional, these observations supplied an essential bridge, implying that pDC overactivation is not a quirk of a model but a feature of treated infection that can be monitored and, potentially, stratified. Together, the cross-system evidence suggested that pDC modulation deserves a seat among candidate strategies for adjunctive therapy. It also flagged crucial guardrails: any clinical application must preserve the early antiviral value of interferon while curbing its chronic, deleterious overhang, a balance that hinges on dosing, timing, and reversibility.
What the Findings Mean for Therapy
Synergy Between Dampening Inflammation And Lifting Exhaustion
A striking thread in the data is the complementarity between trimming back pathogenic inflammation and releasing exhausted T cells from inhibitory checkpoints. pDC modulation alone improved T cell vigor and nudged the reservoir downward, but pairing it with a checkpoint inhibitor amplified the effect, as if removing static and boosting volume together made the clearest sound. Restored stem-like CD8+ T cells appeared better positioned to expand into effectors when needed, and the checkpoint signal helped those effectors sustain activity without immediate relapse into exhaustion. This synergy aligns with broader combination paradigms that target different layers of immune control to achieve more complete, durable responses.
Translationally, the combination model offers a blueprint for building multi-pronged regimens that respect the immune system’s complexity. Rather than assuming a single lever can control viral persistence, the findings argue for targeted stacks: constrain the innate driver that fuels chronic activation, then reinvigorate the adaptive arm to capitalize on the quieter terrain. If validated clinically, such stacks could be layered with other reservoir-directed tools—like broadly neutralizing antibodies or latency-reversing agents—creating a choreography in which timing and sequence matter. The overarching goal is not maximal stimulation but engineered balance that converts temporary boosts into lasting control.
Guardrails, Patient Selection, And Next Steps
The therapeutic promise comes with prudent caveats. pDCs contribute to defense against diverse pathogens and shape vaccine responses, so blunt or prolonged suppression risks unintended openings for opportunistic infections or muted immunogenicity. Any human study will need tight pharmacologic control—time-limited dosing, titratable effects, and clear reversibility—paired with vigilant monitoring of infection markers beyond HIV. Safety boundaries for checkpoint inhibitors also require attention in a population that may already harbor smoldering inflammation; immune-related adverse events must be anticipated and managed with well-defined protocols to avoid trading one imbalance for another.
Future work should prioritize biomarker development to spot individuals with dominant pDC–interferon signatures who may benefit most from targeted dampening. Companion diagnostics could guide on-ramps and off-ramps, ensuring intervention during windows when reservoirs are vulnerable and T cells are poised to rebound. Clinical trials ought to explore combinations with therapeutic vaccines, bNAbs, or latency reversal in sequences tuned to maximize synergy while minimizing risk. If successful, this approach could become a modular component of functional cure strategies—deployed for defined intervals, aligned with adjuncts that push or pull the reservoir, and calibrated to protect the long game of immune health rather than chase short-lived peaks.