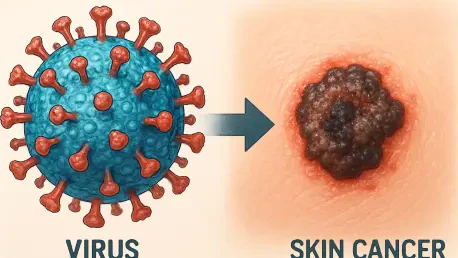
In a stunning revelation that has sent ripples through the medical community, a recent study published in The New England Journal of Medicine has uncovered a direct link between a widespread skin virus and the development of a common form of skin cancer. The research spotlights betapapillomavirus type 19 (beta-HPV), long thought to be a harmless resident of human skin, and its newly identified role in driving cutaneous squamous cell carcinoma (cSCC). This discovery challenges decades of assumptions about the virus’s benign nature and raises urgent questions about its impact on vulnerable populations. Centered on a compelling case of a 34-year-old woman with a persistent forehead tumor, the findings reveal how beta-HPV can integrate into tumor DNA and fuel cancer growth when the immune system is compromised. With skin cancers like cSCC affecting millions annually in the United States, this breakthrough underscores the need to rethink prevention and treatment approaches, potentially transforming how clinicians address these pervasive conditions.
Unraveling the Viral Connection to Skin Cancer
Redefining a Familiar Virus
The perception of beta-HPV as a harmless component of the skin’s microbial landscape has been fundamentally altered by this groundbreaking research. Unlike its more notorious relatives, such as alpha-HPV strains linked to cervical cancer, beta-HPV was largely overlooked as a potential threat. However, the study documents a striking instance where beta-HPV type 19 embedded itself into the DNA of a skin tumor, actively contributing to its growth. This integration mirrors mechanisms seen in other virus-driven cancers, suggesting that beta-HPV can shift from bystander to instigator under specific circumstances. Such a shift in understanding compels the medical field to reassess the risks posed by seemingly innocuous viruses, especially in populations where standard defenses might falter. The implications of this finding extend beyond a single case, hinting at a broader, previously unrecognized role for beta-HPV in oncology.
This redefinition also brings to light the conditions under which beta-HPV reveals its cancer-causing potential. The research highlights that immune suppression appears to be a critical factor, as seen in the patient with a rare T-cell deficiency. In a healthy individual, the immune system typically keeps such viruses in check, preventing them from causing harm. Yet, when those defenses are weakened, beta-HPV can exploit the opportunity to drive abnormal cell growth. This insight suggests that the virus’s threat may be limited to specific contexts, but it also raises concerns about how many undiagnosed cases might involve similar dynamics. Identifying at-risk groups and understanding the precise mechanisms of viral integration could become key priorities for researchers aiming to mitigate this newly identified risk.
Impact on Public Health Challenges
Skin cancer, particularly cSCC, represents a significant public health burden, with an estimated 5.4 million cases diagnosed each year in the United States alone. Often underreported in national data, these conditions strain healthcare resources and affect countless lives with their physical and emotional toll. The revelation that a common virus like beta-HPV could play a direct role in some of these cases adds a layer of complexity to an already pressing issue. It suggests that current strategies focused primarily on ultraviolet (UV) exposure as the main risk factor might be incomplete. Incorporating viral drivers into the broader narrative of skin cancer causes could reshape public health campaigns, emphasizing the need for comprehensive risk assessments that go beyond traditional factors.
Moreover, this finding prompts a reevaluation of preventive measures and early detection protocols. If beta-HPV contributes to cancer in even a subset of cases, screening for viral presence in high-risk individuals could become a valuable tool. Public health officials might also consider educating both clinicians and the general population about the potential dangers of common viruses under specific conditions. While the full scope of beta-HPV’s impact remains unclear, this study serves as a wake-up call to address gaps in understanding and to prioritize research into virus-related cancers. Such efforts could ultimately reduce the incidence of cSCC and improve outcomes for those most vulnerable to its effects.
Immune Dynamics and Therapeutic Breakthroughs
The Pivotal Role of Immune Surveillance
At the heart of this study lies a profound insight into the immune system’s role in preventing cancer, particularly through the function of T-cells. The patient in question suffered from a rare genetic defect that impaired T-cell activation, leaving her body unable to combat the beta-HPV infection or halt the resulting tumor growth. This deficiency created an environment where the virus could persist unchecked, directly sustaining the cancer’s progression. The case vividly illustrates how integral immune surveillance is to maintaining cellular health, acting as a frontline defense against both infections and malignancies. Without effective T-cells, even a typically benign virus can become a dangerous catalyst for disease, highlighting a critical vulnerability in certain individuals.
The implications of this immune dysfunction extend to a broader understanding of cancer development across various contexts. While most people’s immune systems can suppress potential threats like beta-HPV, those with compromised immunity—whether due to genetic conditions, medical treatments, or other factors—face heightened risks. This study underscores the need to identify such vulnerabilities early, as they can profoundly influence disease outcomes. It also emphasizes that addressing cancer may require looking beyond the tumor itself to the systemic conditions that allow it to thrive. Future research might focus on mapping these immune interactions more precisely, offering new ways to predict and prevent virus-driven cancers in susceptible populations.
A Transformative Treatment Outcome
A remarkable turning point in the patient’s journey came with an allogeneic hematopoietic stem cell transplant (HSCT), which effectively restored her immune function. Following the procedure, not only did the tumor regress, but the associated viral conditions also resolved, providing compelling evidence of the link between immune health and cancer control. This outcome suggests that rebuilding immunity can directly address the root causes of certain cancers, rather than merely managing their symptoms. For patients with similar profiles—those with recurring tumors and underlying immune deficiencies—this approach could represent a lifeline, shifting the focus of treatment from reactive to restorative strategies.
The success of the stem cell transplant also points to the potential of immune-based therapies as a frontier in cancer care. While such interventions are not yet standard for cSCC, this case aligns with the growing trend of leveraging the body’s natural defenses through treatments like immunotherapies. It raises the possibility that similar techniques could be adapted for other virus-related cancers, particularly in cases resistant to conventional methods. However, the complexity and risks of procedures like HSCT mean they are not universally applicable, necessitating careful patient selection and further clinical exploration. This breakthrough serves as a proof of concept, inspiring hope for innovative solutions tailored to individual needs.
Future Directions in Research and Care
Tailoring Treatments for Better Outcomes
The insights from this study pave the way for a more personalized approach to managing cSCC, particularly in patients with immune challenges. For those with aggressive or recurring tumors, testing for viral involvement like beta-HPV integration could become a critical diagnostic step. Traditional treatments such as surgery or radiation often fail to address underlying factors, leading to repeated relapses. By identifying a viral driver, clinicians might pivot to strategies that target both the virus and the immune dysfunction, potentially combining antiviral agents with immune-boosting therapies. Such precision medicine could significantly enhance treatment efficacy, offering a more holistic path to remission for select patients.
Additionally, this tailored approach highlights the importance of integrating multidisciplinary care into cancer management. The patient’s outcome was the result of collaboration across virology, immunology, oncology, and transplant medicine, demonstrating how diverse expertise can converge to solve complex cases. Hospitals and research institutions might take note, fostering similar interdisciplinary teams to tackle challenging diagnoses. While personalized treatments are resource-intensive, their potential to improve long-term outcomes justifies investment in developing protocols and technologies that support individualized care. This shift could redefine standards of practice for skin cancer over time.
Exploring the Broader Impact of Beta-HPV
One of the most pressing questions arising from this research is the true prevalence of beta-HPV-driven skin cancer, especially among immunocompromised populations. The current findings are based on a single, unique case, leaving the broader scope of the virus’s impact unknown. Larger, population-based studies are essential to determine how often beta-HPV acts as a cancer driver and under what conditions it poses the greatest risk. Such research could uncover patterns that inform risk stratification, helping clinicians identify who might benefit most from targeted interventions. The urgency of this work cannot be overstated, as it could fundamentally alter the understanding of skin cancer’s causes.
Furthermore, the potential for new therapeutic avenues is a compelling reason to expand research efforts. If beta-HPV’s role is confirmed in wider groups, developing antiviral therapies or immune-modulating treatments could complement existing options. Clinical trials exploring these possibilities might yield innovative solutions, from drugs that inhibit viral activity to vaccines preventing beta-HPV’s cancer-causing effects. Collaboration between academic institutions, pharmaceutical companies, and public health entities will be crucial to drive this progress. The journey from a singular discovery to widespread application is long, but it holds promise for reducing the burden of skin cancer in the years ahead.
Building on Preventive and Collaborative Foundations
Drawing Inspiration from Existing Prevention Models
The success of vaccination programs targeting other HPV strains offers a powerful lesson for addressing beta-HPV’s potential threat. While current vaccines focus on alpha-HPV types linked to cervical cancer, their impact on reducing disease rates demonstrates the value of upstream interventions. Should future studies confirm beta-HPV’s role in a significant number of skin cancer cases, similar preventive strategies could be explored. Developing a vaccine or other preventive measures might one day shield high-risk individuals from the virus’s cancer-causing effects, mirroring the transformative impact seen in other virus-related cancers. This possibility, though distant, underscores the importance of proactive public health measures.
Beyond vaccines, raising awareness about the risks of common viruses in specific contexts is a critical step. Many clinicians and patients remain unaware of beta-HPV’s potential to drive cancer, particularly in immunocompromised individuals. Educational initiatives could bridge this gap, ensuring that healthcare providers consider viral factors in stubborn or atypical cases of cSCC. Public campaigns might also empower individuals to seek screenings if they fall into high-risk categories. By fostering a culture of vigilance and informed decision-making, the medical community can better position itself to catch and address virus-driven cancers early, potentially saving lives through timely action.
The Strength of Interdisciplinary Innovation
The remarkable outcome of this case owes much to the collaborative spirit of the research team, which brought together specialists from diverse fields to solve a complex puzzle. Virologists, immunologists, oncologists, and transplant experts combined their knowledge to not only treat the patient but also uncover a groundbreaking link between beta-HPV and cSCC. This model of integrated effort serves as a blueprint for addressing other multifaceted health challenges, where single-discipline approaches often fall short. Institutions might consider prioritizing such teamwork in future projects, recognizing that innovation often emerges at the intersection of varied perspectives.
Moreover, this collaborative success highlights the need for sustained investment in medical research that crosses traditional boundaries. Funding interdisciplinary studies can accelerate discoveries, as seen in this instance where a single patient’s story reshaped understanding of a common virus. Policymakers and healthcare leaders should take note, advocating for resources that enable such partnerships. By building on this foundation, the medical field can tackle the unknowns surrounding beta-HPV and other emerging threats, ensuring that today’s breakthroughs lay the groundwork for tomorrow’s solutions.