The field of immunotherapy has witnessed a groundbreaking advancement with the introduction of TRACeR-I, a novel protein platform designed to enhance antigen recognition. This innovative platform promises broad HLA compatibility, significantly improving immune response engineering and targeting disease-specific antigens. The study delves into the molecular structure and potential applications of TRACeR-I, emphasizing its role in the targeted recognition of antigen-MHC complex reporter for MHC I.
The Importance of MHC I-Peptide Presentation
Role in Immune Responses
MHC I-peptide presentation is crucial for facilitating immune responses. Diseased cells often accumulate abnormal proteins, such as tumor-associated antigens or neoantigens, alongside pathogen-derived antigens. These proteins are degraded within proteasomes and lysosomes, with some peptide fragments being presented on the cell surface by class I major histocompatibility complex (MHC I) proteins. This presentation enables innate immune cells to mediate the killing of diseased cells and activates adaptive immunity, involving T-cells recognizing antigens, leading to cell-mediated killing and antibody production. Without this essential process, the immune system would struggle to identify and combat cells exhibiting pathogenic or cancerous behaviors.
The presentation of peptides on MHC I also plays a critical role in engaging CD8+ cytotoxic T lymphocytes (CTLs), which are vital for the destruction of infected or abnormal cells. These interactions form the backbone of immunological surveillance and clearance of altered self-cells. The highly specific binding between the T-cell receptor (TCR) on CTLs and the peptide-MHC I complex ensures precision in targeting, enabling effective removal of cells harboring detrimental antigens. However, this specificity is also a double-edged sword, as it complicates the broad applicability of immunotherapies targeting diverse and mutable antigenic landscapes.
Challenges in TCR Engineering
A significant component of the study highlights the potential of T-cell receptors (TCRs) in targeting specific antigens. TCRs achieve specificity by binding to peptide-MHC complexes (pMHC) using six flexible complementarity-determining region (CDR) loops. However, engineering TCR CDRs to create MHC I binding molecules specific to disease antigens poses several challenges. One major issue is the slow development of TCRs from cells with low antigen affinity. Additionally, TCRs exhibit inherent polyspecificity, which limits their specificity as therapeutic agents. Furthermore, the HLA genes encoding MHC I peptides have over 38,000 allotypes, restricting TCRs to pMHC targets across only a few HLA versions.
These challenges underscore the complexity of designing precise TCR-based therapies. The necessity for high-affinity interactions often requires significant modifications of the TCR structure, which can lead to off-target effects and increased immunogenicity. Moreover, the diverse genetic background of patients, represented by various HLA alleles, means that a single TCR-based therapy may not be effective across the entire population. This genetic variability demands carefully tailored approaches that can adapt to individual HLA profiles, further complicating the development process and limiting the speed and scalability of bringing effective therapies to clinical use.
The Breakthrough of TRACeR-I
Overcoming Traditional TCR Limitations
The breakthrough presented in the article lies in the development of TRACeR-I, a platform designed to overcome the limitations of traditional TCRs. TRACeR-I leverages the limited number of backbone conformations on MHC I antigens to create a platform compatible with a wide range of HLA allotypes. This innovation allows a single docking orientation, adaptable to most binders if it covers the full length of the antigen, facilitating cost-effective and rapid production of MHC I binders specific to various disease-related peptides. This flexibility is a significant advance, addressing one of the major bottlenecks in TCR-based therapeutic development.
By simplifying the design to accommodate broad HLA compatibility, TRACeR-I enables more effective targeting of peptide-MHC I complexes across different individuals. This uniformity reduces the need for extensive customization and speeds up the development timeline for new immunotherapies. The ability to produce MHC I binders quickly and cost-effectively opens new avenues for personalized medicine, particularly in conditions with rapid mutation rates, such as cancers and viral infections. Ultimately, TRACeR-I presents an opportunity to create more universally applicable therapies, enhancing the overall effectiveness of immune-based treatments.
Scaffold and Computational Modeling
The scaffold of TRACeR-I is based on a modified version of the previously developed peptide-focused pMHC II-binding platform, TRACeR-II. TRACeR-II features a concave surface that binds perpendicular to the peptide-binding groove on the extended peptide structures of MHC II. By introducing a directed mutation, the research team adapted this platform to engage the bulged peptide conformation on MHC I in a parallel orientation. Computational modeling was employed to identify a sequence compatible with the MHC I surface, followed by variations within the concave feature to optimize the binding mode.
This approach allowed researchers to fine-tune the interface of TRACeR-I, ensuring strong and specific interactions with various MHC I-presented peptides. The utilization of computational tools facilitated rapid iterations and refinements, resulting in a robust platform capable of accommodating different antigenic structures. By focusing on the uniformity of the MHC I binding site, TRACeR-I effectively circumvents the issue of HLA diversity, paving the way for a new class of immunotherapeutics that are both versatile and highly specific.
Testing and Efficacy of TRACeR-I
Binding Specificity and Versatility
The binding specificity of TRACeR-I was thoroughly tested against three distinct pMHC I targets: peptides derived from esophageal squamous cell carcinoma, Epstein-Barr virus, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). These targets were presented on HLA targets across both HLA A02 and B08 allotypes. The results demonstrated that TRACeR’s peptide-focused binding interface specifically bound all three targets, suggesting a generalized binder-generating platform capable of targeting multiple HLA alleles. The versatility of TRACeR-I indicates that it can bind to a wide range of targets across different populations, highlighting its potential in various applications.
The success of these tests underscores the potential of TRACeR-I in various therapeutic scenarios. Its ability to target peptides from a range of diseases represents a significant leap forward in immunotherapy. By binding effectively to diverse pMHC I presentations, TRACeR-I could become a fundamental tool for developing treatments for cancers and infectious diseases. Moreover, its compatibility with multiple HLA allotypes ensures that therapies based on this platform could be accessible and beneficial to a broader patient population, addressing a critical need for inclusivity in medical treatments.
Safety and Efficacy in Preclinical Models
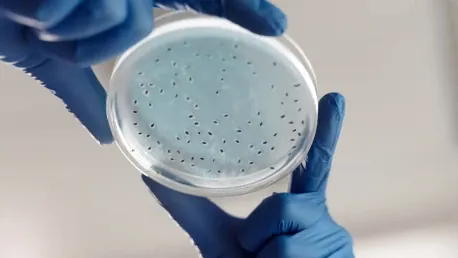
Notably, despite their bacterial origin, TRACeRs did not provoke significant immune or cytotoxic responses in mice, underscoring their potential safety and efficacy. To further investigate the efficacy of TRACeR-I, the platform was incorporated into a humanized antibody fragment in a bispecific T-cell engager (BiTE) format. When tested against patient-derived cancer cells, it effectively activated T-cells and induced on-target killing at nanomolar concentrations. The detailed examination of the molecular mechanism through X-ray crystallography revealed that TRACeR engages the pMHC I target along its entire length by shape complementarity.
The preclinical success of TRACeR-I shows significant promise for future clinical applications. The ability to integrate into existing therapeutic formats, such as BiTEs, and to elicit a precise T-cell response at minimal concentrations, underlines its potential for real-world use. The findings from X-ray crystallography provide detailed insights into the interactions at the molecular level, reinforcing confidence in the platform’s robustness. With a solid foundation in preclinical models, TRACeR-I stands poised to transition into clinical trials with a strong safety and efficacy profile, potentially revolutionizing the way immunotherapies are developed and administered.
Future Directions and Potential Applications
Broad Compatibility and Development Processes
The field of immunotherapy has experienced an innovative breakthrough with the release of TRACeR-I, a state-of-the-art protein platform aimed at enhancing antigen recognition capabilities. This pioneering platform is notable for its extensive HLA compatibility, which marks a significant stride in refining immune response engineering and accurately targeting disease-specific antigens. The detailed research examines the molecular structure of TRACeR-I and explores its wide-ranging applications. Highlighting its crucial role, the study focuses on TRACeR-I’s capability to facilitate targeted recognition of antigen-MHC complex reporters for MHC I. This advancement heralds potential improvements in immunotherapy treatments, offering a more precise approach to identifying and combating diverse diseases by improving how immune cells recognize and attack harmful antigens. The implications of TRACeR-I’s broad compatibility could revolutionize targeted therapies, making treatments more effective and personalized to individual patients’ needs.