The development of synthetic intramembrane proteolysis receptors (SNIPRs) engineered by researchers in the United States could be a game-changer for CAR T-cell cancer therapies. This groundbreaking advancement introduces a novel methodology to enhance the precision and safety of CAR T-cell treatments, which have traditionally been plagued by weak responses and potential off-target effects. The study, published in the journal Nature, presents the creation of SNIPRs that activate therapeutic cells in response to soluble ligands with remarkable sensitivity and specificity.
Background of CAR T-Cell Therapies
Traditional CAR T-Cell Limitations
Cells’ ability to detect and respond to soluble molecules is fundamental to complex biological functions such as immune responses and tissue development. Synthetic biology seeks to replicate these capabilities for therapeutic applications, including engineering cells to respond to specific signals or communicate via artificial pathways. However, the current receptor systems, including traditional CAR T-cells, face significant hurdles. These challenges encompass limited ligand flexibility and overly complex multi-component designs, which complicate clinical applications.
Traditional CAR T-cell therapies often show weak responses in targeting specific cells and pose a risk of off-target effects, which can sometimes result in the immune system attacking healthy tissues. This inherent limitation necessitates developing a more advanced receptor system that can offer higher precision and sensitivity in detecting cancer cells, thus enhancing overall treatment effectiveness and patient safety. The imperative need for improved precision drives ongoing research in developing sophisticated therapeutic platforms.
Need for Enhanced Precision
The desire to refine CAR T-cell therapies is almost entirely driven by the goal of achieving improved therapeutic outcomes while reducing adverse effects. Traditional CAR T-cells encounter multiple challenges, which include weak responses to target cells and the risk of attacks on healthy tissues. These obstacles highlight the critical need for more sophisticated receptor systems that can provide a higher level of specificity and sensitivity in targeting cancer cells.
The quest for enhanced precision in CAR T-cell therapies aims to ensure the treatments are not only more effective but also safer for patients. A sophisticated receptor system capable of discerning between healthy and cancerous tissues can significantly improve therapeutic outcomes. This would enable more precise targeting of malignant cells, minimizing the potential for off-target effects, and potentially extending the applicability of CAR T-cell therapies beyond cancer into other diseases requiring targeted cellular responses.
Development of SNIPRs
Notch-Based Architecture
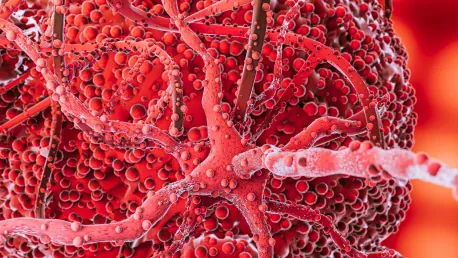
Researchers have developed SNIPRs by utilizing a Notch-based architectural design to address the hurdles faced by traditional CAR T-cell therapies. These compact, single-chain receptors have a distinctive ability to detect soluble ligands through ligand-triggered dimerization followed by endosomal signaling. This mechanism allows SNIPRs to bypass the mechano-sensing filters used by conventional methods, leading to potent and precise activation of therapeutic genetic programs within immune cells.
SNIPRs stand out from other receptor systems, such as synNotch receptors, due to their unique ability to operate through endosomal signaling pathways instead of relying on surface-mechanistic interactions. This distinction is critical because it equips SNIPRs with the capacity to robustly detect and respond to soluble factors, ensuring highly accurate targeting of the desired cells. This innovative approach substantially mitigates the risks associated with off-target effects, making the therapy safer and more effective for patients.
Engineering and Optimization
SNIPRs were skillfully engineered to detect tumor-associated cytokines, such as TGF-β and VEGF, utilizing single-chain variable fragments (scFvs) derived from antibodies. These engineered receptors were integrated into human CD3+ T-cells and optimized by modifying the properties of the scFv and the hinge domains. Adjustments, such as the mutation of cysteine residues to serine in the hinge domains, enhanced the receptors’ sensitivity while minimizing background activation. Furthermore, the performance of SNIPRs was finely tuned using inhibitors like DAPT and chloroquine.
The engineering and optimization process extended to improving the overall efficacy and specificity of SNIPRs. Fine-tuning these receptors to achieve the desired sensitivity levels allowed them to reliably detect and respond to tumor-associated cytokines. This optimization included careful adjustments to the structural components of SNIPRs and the use of chemical inhibitors, which enhanced their therapeutic performance. These efforts have resulted in a receptor system that holds significant promise for advanced cellular therapies due to its precise targeting capabilities and minimized risk of non-specific activation.
Experimental Findings
In Vitro Analysis
Extensive in vitro analysis demonstrated that SNIPRs effectively activate transcriptional programs in human T-cells upon ligand binding. Modifications to the scFv, orientation, and transactivation domains played a crucial role in enhancing both potency and specificity. In addition, SNIPRs showcased the potential to detect additional soluble factors, such as fibroblast growth factor 2 and interferon-γ. This ability offers a controlled “private” communication channel for engineered cells, significantly expanding the versatility of SNIPRs for various therapeutic applications.
SNIPRs’ capability to precisely detect and respond to multiple soluble factors underscores their potential for use in sophisticated therapeutic strategies. By providing a controlled communication channel, these receptors can be tailored to discern specific signal molecules, ensuring targeted activation for therapeutic purposes. This versatility makes SNIPRs an invaluable tool in cellular therapy development, potentially transforming how doctors approach the treatment of various diseases, including cancer and autoimmune disorders.
Endocytic Activation Pathway
Activation by SNIPRs involves an endocytic pathway where ligand binding triggers internalization and subsequent proteolysis. This was confirmed through confocal imaging, showing ligand-receptor co-localization within internal cellular compartments. Additionally, experiments with synthetic ligands featuring modified valencies and geometries demonstrated the tunable nature of SNIPRs’ responses, allowing fine control over signaling strength and timing, which is crucial for precise therapeutic interventions.
The utilization of an endocytic pathway for SNIPR activation represents a significant departure from traditional receptor systems. This approach ensures that the signal from the ligand binding is amplified through internal proteolytic processes, resulting in robust and accurate activation of the intended genetic programs. The ability to tune SNIPR responses further highlights their flexibility and adaptability, allowing researchers to control and refine signaling strength and timing to optimize therapeutic outcomes. This precision is essential in ensuring the safety and efficacy of targeted therapies, offering a significant improvement over current methods.
In Vivo Analysis
Tumor Cell Killing
In vivo analysis revealed that SNIPRs displayed dose-dependent responses to soluble factors such as TGF-β1 and VEGFα. These responses correlated with ligand production, indicating the effectiveness of SNIPR activation in real biological environments. Additionally, SNIPR → CAR circuits exhibited remarkable tumor cell-killing capabilities, particularly against Her2-specific CARs. While these circuits demonstrated slower kinetics due to delayed CAR expression, their exceptional specificity showcased their potential as a superior therapeutic option.
The successful demonstration of SNIPR-mediated tumor cell killing in vivo confirms their efficacy as a therapeutic tool. The ability to generate dose-dependent responses ensures that therapeutic interventions can be carefully regulated, minimizing the risk of excessive immune activation. The specific targeting of tumor cells without harming healthy tissues enhances the safety profile of SNIPR → CAR circuits, potentially improving clinical outcomes for patients undergoing CAR T-cell therapy. These promising results pave the way for further research and clinical trials to establish the full potential of SNIPRs in cancer treatment.
Mouse Model Studies
Mouse model studies further underscored the advantages of SNIPR → CAR circuits over conventional CAR-T approaches. In models with melanomas and lung adenocarcinomas, SNIPR → CAR circuits demonstrated improved safety and efficacy, reducing severe off-target effects and optimizing therapeutic windows. These results signify the potential of SNIPRs to enhance the precision and effectiveness of CAR T-cell therapies in living organisms, offering a revolutionary approach to cancer treatment.
The integration of SNIPRs into mouse model studies highlighted their capability to improve the therapeutic potential of CAR T-cell therapies significantly. The reduction in off-target effects is especially crucial, as it enhances patient safety while optimizing the effectiveness of the treatment. These findings have substantial implications for the future of CAR T-cell therapies, suggesting that SNIPRs could lead to more successful and safer cancer treatments. The promising results in preclinical models warrant further investigation and potential translation into human clinical trials to fully explore the benefits of this innovative approach.
Broader Implications and Future Directions
Integration with Bioengineering
The broader implications of SNIPRs extend well beyond cancer therapy, potentially revolutionizing other fields such as tissue engineering, developmental biology, and autoimmunity research. Their high sensitivity and modularity make them well-suited for integration into complex biocomputational circuits and multi-receptor systems, allowing precise control of cellular behavior. This adaptability equips SNIPRs for diverse biological contexts, enabling the design of highly accurate and responsive therapeutic strategies for a range of medical applications.
SNIPRs’ ability to detect and respond to signaling gradients opens new possibilities in tissue engineering, where precise control over cellular responses is crucial. Additionally, their potential to contribute to developmental biology research offers insights into complex developmental processes, providing new avenues for studying and possibly rectifying developmental disorders. In autoimmunity research, SNIPRs’ targeted detection capabilities can help design therapies that modulate immune responses more accurately, minimizing the risk of unintended immune activation. The flexibility and responsiveness of SNIPRs make them a promising tool for various scientific and medical fields.
Enhancing Targeting Precision
Enhancing the targeting precision of SNIPRs further is a primary focus for future studies. This involves optimizing SNIPRs’ response profiles through hinge domain engineering or integrating them with multireceptor circuits to cater to dynamic tissue environments. Researchers are also exploring the potential for dual activation by soluble and membrane-bound ligands, which can refine targeting within microenvironments. Integrating SNIPRs with multi-cell signaling networks can lead to advanced therapeutic strategies that offer unprecedented control over cellular functions and therapeutic responses.
As research progresses, the fine-tuning of SNIPRs’ targeting precision will likely lead to more sophisticated and effective therapies. The ability to dual-activate SNIPRs through different ligand types holds particular promise, allowing for more nuanced and context-specific therapeutic interventions. By integrating SNIPRs into multi-cell signaling networks, researchers can create more complex and dynamic therapeutic strategies tailored to specific patient needs. This approach has the potential to revolutionize personalized medicine by providing highly customizable and precise treatment options that adapt to the unique characteristics of each patient’s disease.
Conclusion
Researchers in the United States have developed synthetic intramembrane proteolysis receptors (SNIPRs) which could revolutionize CAR T-cell cancer therapies. This significant innovation presents a new approach to increase the accuracy and safety of CAR T-cell treatments, addressing common issues like weak responses and potential off-target effects that have traditionally hampered these therapies. The study, published in the prestigious journal Nature, showcases the engineering of SNIPRs designed to activate therapeutic cells upon detecting soluble ligands, demonstrating remarkable sensitivity and specificity. These SNIPRs represent a breakthrough in enhancing the precision of CAR T-cell therapy, as they enable the activation of therapeutic cells only in the presence of specific signals. This minimizes unintended consequences and improves the overall treatment effectiveness and patient safety. By honing in on these precise signals, SNIPRs offer hope for more targeted cancer treatments, potentially transforming the landscape of immunotherapy and providing better outcomes for patients.