The recent COVID-19 pandemic undoubtedly reshaped healthcare systems around the world, while also increasing the pressure to develop and deliver better vaccines and treatments. Biopharmaceutical companies everywhere raced to find the first vaccine and the most effective drug as the healthcare crisis continued to intensify. However, although vaccines and treatments for COVID are now widely available in most countries, the crisis is far from over for biopharma companies that focus on research and development. Long-term effects, known as long COVID, is just one of the reasons why they need to continue their work.
According to the Center for Disease Control and Prevention (CDC), some people who have previously suffered from COVID can develop lasting effects as a consequence of the disease. These long-term symptoms are known as post-COVID conditions (PCC) or long COVID. People with long COVID commonly report general symptoms such as tiredness, fatigue, fever, more specific respiratory and heart symptoms—such as trouble breathing or palpitations—and neurological issues, such as a lack of mental clarity or migraines, digestive symptoms, and more. However, although several people are currently suffering from symptoms associated with long COVID, no test can be used to diagnose this condition.
One in five Americans who contracted COVID-19 are suffering from long COVID symptoms according to the CDC. The agency cites data from the Household Pulse Survey, which also mentions that more than 40% of American adults reportedly had COVID-19.
Trying to Find the Right Treatments
According tо CBS News, long COVID remains one of the biggest mysteries of the recent healthcare crisis. Experts in the US and abroad are still trying to answer important questions about the condition, such as why some individuals report debilitating symptoms that linger for months after COVID, and what treatments and cures could be used to alleviate their symptoms.
More than 26 trials have been launched to test long COVID treatments according to Nature magazine. While some drugs and therapies are designed to alleviate inflammation and prevent the formation of blood clots, treatments like Fluvoxamine aim to reduce neuropsychiatric symptoms like headaches, fatigue, anxiety, or depression. Scientists are now trying to repurpose drugs like Fluvoxamine to treat long COVID symptoms. Previous studies demonstrated that this drug was useful in preventing hospitalization during the initial COVID-19 pandemic, and scientists now hope it could prove effective once again.
However, it is worth noting that the US Food and Drug Administration (FDA) recently rejected an emergency use authorization request for Fluvoxamine—a drug that has been designed to treat obsessive-compulsive disorder (OCD).
Hopes Rise as October Approaches
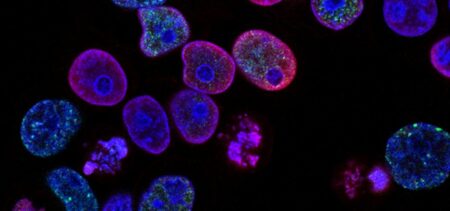
Although various trials and studies are already underway in the US and abroad, scientists hope that the new RECOVER initiative will ultimately shed some light on long COVID’s wide range of lingering symptoms. The initiative was created to understand how and why some people completely recovered from the disease, while others continued to develop symptoms associated with long COVID. Scientists hope to collect new data about the long-term effects of COVID so they can develop new preventive methods and treatments.
More than 8,000 Americans enrolled in RECOVER studies, but researchers say that more volunteers are needed. However, with policymakers, supporting organizations, caregivers, researchers, and healthcare providers now also participating in these studies, more American volunteers are bound to join. According to Dr. Walter Koroshetz (Director of the National Institute for Neurological Disorders and Strokes and promoter of the new RECOVER initiative) the final months of 2022 may be the beginning of “something big” in COVID research.
Conclusion
Big or small, new research is needed to better understand what long COVID really is and how it could be treated effectively in the future. The good news is that scientists, healthcare providers, and biopharmaceutical companies are now joining forces to do exactly that.